What the Dental Professional Must Know About Bisphosphonate Medications
Reviewing our patients’ medical histories has just gotten more critical than ever before. Too often we ask breezily if there have been any changes in the patient’s health, and accept the standard “no” without delving further. Patients do not understand the connection between the medications they take for various health issues and the treatment they receive in the dental office. For this reason, they respond in the negative because it’s easier than listing medications. They may also feel it is an invasion of their privacy for us to ask questions about their medical health when all they are here for is “a simple dental cleaning.”
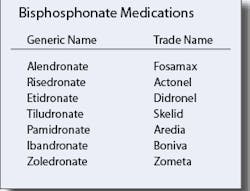
The fact is, our patients’ health may be vitally affected if we proceed with dental treatment without knowledge of the medications they are taking. The newest medications to result in devastating dental effects are the bisphosphonates.
In the dental office, we see hundreds, possibly thousands, of patients annually who are taking oral bisphosphonates for osteopenia and osteoporosis. The majority of these patients are Caucasian women of slight build, but men take this medication as well. Bisphosphonates are widely advertised on television and in consumer magazines. Doctors prescribe them by the millions. The impression to the general public is that they are safe and effective against the dreaded disease, osteoporosis. While they are effective, they are not without great risk.
The dental risk that we must be aware of is osteonecrosis, or death of the jawbone. “Osteonecrosis of the Jaw (ONJ) has been reported in patients with cancer who are receiving treatment including bisphosphonates, chemotherapy, and/or corticosteroids. The majority of reported cases have been associated with dental procedures such as tooth extraction. A dental examination with appropriate dentistry should be considered prior to treatment with bisphosphonates in patients with concomitant risk factors. While being treated with these medications, patients should avoid invasive dental procedures if possible. No data is available as to whether discontinuation of bisphosphonates therapy reduces the risk of ONJ in patients requiring dental procedures.” (http://www.us.aometa.com/hcp/safetyinformation.jsp.)
Bisphosphonate medications act as bone resorption inhibitors, which increase bone density by binding to the bone matrix and slowing down osteoclastic (bone-destroying) activity, thereby facilitating osteoblastic (bone-building) effectiveness.
This action may help prevent fractures in the hip, spine, and other skeletal regions, but it may disrupt the osteoclast and osteoblast axis in the jaws, impairing osteoclasts’ ability to remove and thus repair or contain diseased bone. This impairment causes osteoblasts to overbuild or wall off diseased bone. As osteoblasts build new bone, the failure of osteoclasts to remove contaminated bone interferes with the development of the necessary structure on which to lay down healthy bone.
Bisphosphonates irreversibly alter the metabolism of the osteoclasts, so there is little or no bone resorption, even if the blood supply is good. The action of bisphosphonates that dental professionals should be concerned about is that they destroy osteoclasts, without which there is no bone healing.
Osteonecrosis of the jaw is also known as avascular necrosis of the bone, or osteochondritis dissecans (the death of bone resulting in the collapse of the bone’s structural architecture). It leads to bone pain, loss of bone function, and bone destruction, and it is the result of a number of conditions leading to an impairment of the blood supply to the bone. Symptoms of ONJ also include toothache, exposed bone, swelling and loosening of the teeth, altered sensation, and recurrent soft-tissue infection. ONJ frequently results in chronic pain and disfigurement, and it is difficult to treat.
The IV forms of the bisphosphonate medications have proven to have the most devastating effects, but the oral forms are also implicated in osteonecrosis. Both the IV and oral forms have the same mechanism of action.
The jawbone is particularly vulnerable to osteonecrosis because of tooth and gum susceptibility to infection. The risk factors for developing osteonecrosis of the jaw include:
It is important to note that withdrawing the medication is not thought to make any difference in the outcome. Bisphosphonates have a 10-year half-life and will accumulate in the bone for up to three half-lives, or 30 years. For the next 30 years, a patient who once received bisphosphonate therapy may be at significantly increased risk for osteonecrosis, and dental treatment must be carefully considered. Many general practitioners are referring all such patients to oral surgeons if extraction is necessary.
It is our professional responsibility to be aware of the potentially devastating health effects of dental procedures for patients who are receiving bisphosphonate therapy and to educate our patients to the risks. Start with a thorough medical history update. Don’t hesitate to contact the patient’s physician(s) for more information if you feel it is in your patient’s best interest. You may help prevent devastating results. RDH