Some common drugs and the impact on the oral cavity
by Pamela Myers, RDH
Most patients cannot accurately tell you what medications or dosages they are taking, especially geriatric patients. One patient that I recently treated in the private sector, where I occasionally practice, was an 85-year-old World War II veteran. He is very alert and very agile for his age. But when I inquired about his medications, he simply said, "Well, I take something for my thyroid and a couple of diabetes pills, and something for my heart."
I asked him the names and dosages, and he laughingly said, "Well, they are hard to remember ... It would be easier if they just were called Diabetes pill 1 and Diabetes pill 2."
Sound familiar? In my full-time practice, I am blessed in that I provide care with electronic medical records that provide me with my patient's current medications and dosages in real time. However, access to the patient's current medications may not be enough information. Most patients over the age of 50 are taking at least three prescribed maintenance medications. If your patient population is over the age of 65, it could be on average at least four maintenance prescriptions, plus an assortment of other over-the-counter (OTC) supplements.
Maintenance drugs do not include antibiotics, antivirals, or anti-inflammatory/pain medication prescribed for short-term dosages. What I hope to do with this article is to give practicing hygienists a basic overview of oral side effects of the most commonly prescribed medications, as well as some medications that have adverse oral effects that they and their patients should be aware of.
Gingival hyperplasia, overgrowth of the gum tissue, is common in patients taking anticonvulsants, immunosuppressant drugs, and calcium channel blockers taken by cardiac patients.
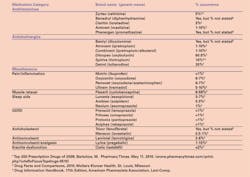
Xerostomia, or dry mouth, is prevalent with antihistamines, anticholinergics, antidepressants/antipsychotics, antihypertensives, diuretics, antiulceratives, central nervous system stimulants (CNS), bronchodilators, and some cancer chemotherapeutic agents (see Table 2).
Increased gingival bleeding may occur in patients taking anticoagulants such as aspirin therapy, Plavix (clopidogrel), or Coumadin (warfarin).
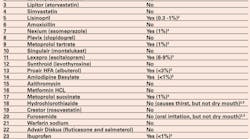
The most commonly prescribed medication classes include contraceptives/hormones, analgesics, antilipemics, antihypertensives, antiulceratives, and antipsychotics/antidepressants (see Table 1).
Hormones and oral contraceptives – Most women of child-bearing age are using a contraceptive. Oral or systemic contraceptives have been available for almost 50 years and are widely used by women between the ages of 15 and 45. They are hormones. The progestin compound in oral contraceptives can cause fatigue, which can adversely affect a patient's oral hygiene compliance – too tired to floss! The estrogen component can cause nausea, which can be accompanied by acid reflux, leading to acid erosion of the tooth enamel.
Most birth control pills are a progestin-only pill commonly referred to as POP or the mini-pill or may be a combination drug containing estrogen and progestin. The POP medications are slightly less effective and can cause nausea or upset stomach, which can result in acid erosion of the enamel if vomiting is a persistent side effect.
Oral soft tissue reactions are not uncommon in females taking oral contraceptives. These may range from slight discoloration to inflammation of the gingival tissue. Most of the time, good home care can significantly decrease the incidence of this problem. If not resolved, the prescribing physician should be consulted and an alternative medication used when possible.
A contraceptive injection is also available, Depo-Provera, which is a synthetic form of progesterone. This injection can prevent pregnancy for 11 to 14 weeks. This drug has a black box warning from the Food and Drug Administration, which states that the "use of Depo-subQ Provera 104 or Depo-Provera may cause you to lose calcium stored in your bones. The longer you use Depo-Provera, the more calcium you are likely to lose. The calcium may not return completely once you stop using Depo-Provera. Loss of calcium may cause weak bones that could increase the risk that your bones might break, especially after menopause. It is not known whether your risk of developing osteoporosis may be greater if you are a teenager when you start to use Depo-Provera. You should only use Depo-Provera long-term (more than two years) if other methods of birth control are not right for you." This could have long-term implications for acerbating bone loss due to periodontal disease.
Premarin and other estrogen-containing medications are prescribed as hormone replacement therapy (HRT) for peri- and postmenopausal women and can cause nausea and vomiting, which can cause enamel erosion.
Antihypertensives – Due to the widespread problem of obesity, we are seeing more younger patients taking antihypertensive medications that can cause xerostomia. Tenormin (atenolol), Toprol XL (metoprolol succinate), Lopressor (metoprolol tartrate), Norvasc (amlodipine), Calan SR (verapamil hydrochloride), Vasotec (enalapril ), Prinivil or Zestril (lisinopril), Cozaar (losartan), Diovan (valsartan), Catapres (clonidine), Lotrel (amlodipine/benazepril), Prinzide or Zestoretic (lisinopril/hydrochlorothiazide) include xerostomia as an adverse reaction (see Table 2).
Coreg and Coreg CR (carvedilol) have been linked to periodontitis and nausea.
Antilipemics – Many patients are taking antilipemics – cholesterol lowering medications. Prescriptions for this class of drug have been steadily increasing in recent years. Zocor (simvastatin), Pravachol (pravastatin), Tricor (fenofibrate), Lipitor (atorvastatin calcium), and Crestor (rosuvastatin calcium) can cause nausea and vomiting.
In addition to nausea, vomiting, and heartburn, Crestor has been linked to periodontal abscess. One side effect of Lovaza® (omega-3-acid ethyl esters) is altered taste, which can result in higher consumption of sweet or salty foods that can contribute to a higher incidence of caries.
Antiulceratives and reflux drugs – Unfortunately, many patients are taking prescribed or other OTC medications for gastroesophageal reflux disease (GERD). Our high stress society and a combination of tobacco usage and/or alcohol exacerbate this problem. GERD can contribute to acid erosion of the enamel, but the medications for GERD can also have oral side effects.
Kapidex (dexlansoprazole) is not as commonly prescribed as other GERD medications. But it can cause altered taste, xerostomia, and halitosis, as well as oral paresthesia.
Nexium (esomeprazole magnesium), Prevacid (lansoprazole), and Prilosec (omeprazole) can cause xerostomia, vomiting, and nausea. These drugs are commonly used to treat acid reflux.
Antihistamines and bronchodilators – Claritin (loratadine), Allegra (fexofenadine hydrochloride), and Zyrtec (cetirizine hydrochloride) are in the antihistimine class of drugs. All antihistimines cause mild to extreme xerostomia. If taken long-term, this class of drugs can contribute a higher caries incidence due to reduced salivary flow.
Ventolin and Proventil (albuterol sulfate) can cause dry throat, altered taste, nausea, and vomiting that may result in increased caries.
Spiriva (tiotropium bromide) is prescribed as a maintenance drug for the treatment of chronic obstructive pulmonary disease (COPD). Spiriva has been linked to xerostomia, GERD, and vomiting. Since this is a maintenance drug, it is used long-term, which can result in the oral side effects occurring throughout the patient's lifetime. Counseling for xerostomia and products to aid with xerostomia should be a part of patient teaching.
Anti-inflammatory and opioid analgesics – Since I now am of the age to feel those aches and pains my parents and grandparents complained of, this class of drug is of more interest to my personal health. I discover more of my patients are taking pain and anti-inflammatory medications for those little aches and pains.
If you treat a geriatric population, you have been very aware of the increase in prescriptions for Celebrex (celecoxib), ibuprofen, NSAIDs, and codeine. Arthritis is not a condition found only in a geriatric population, but is definitely more common in this age group.
Celebrex, NSAIDs, Advil or Motrin, and Indocin (indomethacin) can cause nausea and vomiting, contributing to a higher decay rate. Naproxen prescriptions – Naprosyn, Naprelan, Aleve, and Anaprox – cause stomatitis, dry mouth, nausea, and heartburn. The OTC strength of naproxen sodium, Aleve, can also cause the same oral side effects as the prescription strength.
Methadose (methadone hydrochloride) is used to treat severe chronic pain as well as opioid withdrawal syndrome. This drug can cause nausea, vomiting, glossitis, and xerostomia.
Codeine (codeine phosphate and sulfate) cause xerostomia and nausea.
In 2009, the FDA released a guideline requiring manufacturers of OTC pain relievers, arthritis medications, and fever reducers to revise their package labeling to reflect warnings about liver damage with excessive doses of acetaminophen and internal bleeding with average doses of nonsteroidal anti-inflammatory agents (NSAIDs). When completing a medical history, it is just as important to note OTC medications and supplements as these products may also affect the patient's overall health and the oral cavity.
Antidepressants and antipsychotics – Most antidepressants, antipsychotics, and central nervous system stimulants cause moderate to severe xerostomia. These patients not only have dry mouth, but many times their mental health adversely impacts their oral hygiene and diet (see Table 2).
Osteoporosis and bisphosphonates – No article on oral side effects would be complete without a reference to bisphosphonates. Bisphosphonates are prescribed most commonly for osteoporosis. Osteoporosis is not just something that occurs with age or only in women.
Boniva (ibandronate sodium) as well as other bisphosphonates may cause nausea, vomiting, and GERD, contributing to a higher caries incidence. Bisphosphonates such as Fosamax, Fosamax Plus D, Actonel, Actonel with Calcium, Boniva, and Atelvia list a drug alert for atypical fractures of the femur.
Bisphosphonates may lead to osteonecrosis, mainly of the mandible. Dental surgery or other invasive dental procedures may worsen the condition. Dental providers should consult with the patient's physician regarding consideration for stopping the drug if the patient needs an invasive dental procedure. Only the physician should stop the medication.
Intravenous bisphosphonates – Zometa and Reclast (zoledronic acid) and Aredia (pamidronate disodium) – are prescribed for cancer patients and those with severe osteoporosis not related to cancer or cancer therapy. All of the intravenous bisphosphonates increase the risk of osteonecrosis of the jaw. As a result, the patient's physician should always be consulted prior to performing any invasive dental procedure, including nonsurgical scaling and root planing.
Anticonvulsants – While anticonvulsants are not a more commonly prescribed class of medications, they are important to dental care providers due to their significant oral side effects. Dilantin (phenytoin-diphenylhydantoin) causes gingival hyperplasia. Sometimes the hyperplastic tissue will completely cover the dentition and must be surgically removed.
The FDA recently released a drug warning to clinicians regarding Topamax (topiramate). Topiramate is prescribed for epilepsy and the treatment of migraines. The prevalence of oral cleft palate was significant in infants born to mothers taking topiramate during pregnancy.
"The benefits and risks of topiramate should be carefully weighed when prescribing this drug for women of childbearing age, particularly when topiramate is considered for a condition not usually associated with permanent injury or death." The FDA urged physicians to consider seeking appropriate alternative treatment.
What drugs are in your medicine cabinet? Researching this article piqued my interest and encouraged me to become a "drug detective." My curiosity grew as I searched and read about the side effects of prescribed medications that my elderly parents are taking as well as medications taken by other members of my family and my patients. I encourage all of you to become a "drug detective." Our patients look to us as their dental care expert and we should be a source of useful health information that will result in improved patient outcomes, and better patient overall health and well-being.
Pamela J. Myers, RDH, has been a practicing dental hygienist for 36 years and is currently the Dental Hygiene Program Manager for the University of Texas Medical Branch – Correctional Managed Care in Huntsville, Texas.
References
Health Services Research, 2006, April; 41 (2): 411-428 doi:10.1111/j.1475-6773.2005.00495.x.
Fearing Tornwall R, Pickett FA. FDA Releases New Guidelines for Medication Labeling; Dimensions of Dental Hygiene; Belmont Publications; November 2009, pages 54-57.
Pickett FA and Shargua CR. Addressing Adverse Drug Effects; Dimensions of Dental Hygiene; Belmont Publications; January 2010; pages 38-42.
Most Commonly Prescribed Drugs; Blue Cross and Blue Shield Insurance of Texas, Prime Therapeutics LLC, January 2011.
U.S. Food and Drug Administration.
Medpage Today, LLC; www.medpagetoday.com. Online resource for up to date healthcare information.
Herring PC. Pharmacy Clinical Practice Specialist, University of Texas Medical Branch-Correctional Managed Care.
Nursing Drug Handbook, 2011; 31st Edition; Lippincott. Williams, & Wilkins.
Novartis Oncology Drug Precaution Notice for Aredia and Zometa, Novartis Pharmaceuticals Corporation, One Health Plaza East Hanover, New Jersey.
Hess L, Jeter J, Beham-Hutchins M, Alberts DS. Factors Associated with Osteonecrosis of the Jaw among Bisphosphonate Users; The American Journal of Medicine, Vol. 121, No. 6, June 2008.
FDA Safety Advisories, September through December 2010.
http://www.eda.gov/Safety/MedWatch/default.htm.
The Pill Pass Newsletter, March 2011, published by University of Texas Medical Branch-Correctional Managed Care, Department of Pharmacy.
Past RDH Issues