By Shirley Gutkowski, RDH, BSDH, FACE
How on earth did the words "brush" and "floss" come to define our entire profession? Did we spend almost 3,000 grueling hours learning only how to teach people to brush 'n' floss? I don't think so. What we learned is how to bring the mouth to health. What we learned is more accurately achieved today with probiotics, xylitol, dietary changes, and neurogenesis.
The brain is plastic in that it's moldable and new pathways can be built, which is a process called neurogenesis. Providing the brain opportunities for neurogenesis is important to brain health. It turns out that playing Sudoku doesn't stimulate brain fitness; it helps a person become really good at Sudoku. It is kind of like telling patients to brush 'n' floss the same way over and over -- you become really great at explaining the mechanical removal of plaque.
To start your own neurogenesis mission, stop the brush 'n' floss default story. Focus on the term biofilm management. Learn about and then talk to your patients about biofilm. Then talk about how oral probiotics can reduce oral biofilm, particularly in the secret spots where a brush and floss cannot reach. All probiotics work in the digestive system, but few can function in the first six inches of the mouth.
Oral probiotics
Oral probiotics are a little different than their counterparts. Probiotics for the gut must make it past the hostile environment of the stomach. For example, yogurt is teeming with excessive numbers of live bacteria. This is so an appropriate number of live bacteria can make it to the intestines where they can do their work. Probiotic tablets are specially coated to help them stay together until they get to the right part of the digestive system, where the friendly bacteria are released.
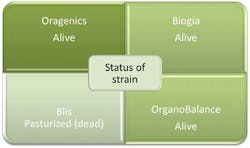
Oral probiotics must be activated in the mouth. Most people immediately think that the tablets or capsules are teeming with motile bacteria. Not so. The bacteria are freeze-dried so that they can reanimate under moist conditions (see Figure 1).
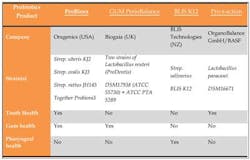
Strains of oral bacteria should be in oral probiotics. Many contain strains that come from other parts of the digestive system or even from dairy products (see Figure 2). An online search for oral probiotics finds a number of products that should raise some questions -- what part of the body did the strains come from, what's their function, and what else is in there (see Figure 3)? Companies that support oral health are adding xylitol to their probiotic products.
Unless there's a specialized manufacturing process that isolates the freeze-dried bacteria from the xylitol moisture contamination, concerns are high. Xylitol is hygroscopic, one of the specialized and under-published features of xylitol. That's not a typo, the word is not hydroscopic. Hygroscopic ingredients attract water, or more accurately, moisture. In the world of oral probiotic stabilization, moisture is a no-no because it may hydrate the freeze-dried bacteria. Just adding xylitol doesn't make the oral probiotic lozenge better or even good. Keep asking yourself -- how much room does a germ need, and how much moisture does it take to reanimate a freeze-dried germ? The answer is, less than an oral health-care provider can measure with a periodontal probe.
The people at Oragenics have found a way to isolate the freeze-dried active ingredient and separate it from the xylitol sweetener. They're continually looking for other ways to provide patients with the blend of naturally occurring oral bacteria.
Naturally altering oral pH
Oral probiotics and gut probiotics share a health goal. To achieve that goal they use health-promoting bacteria to crowd out the disease-promoting bacteria. That's how the oral probiotics, such as ProBiora3 in the Evora brand of oral probiotics, work. The ProBiora3 complex is a grouping of early biofilm colonizers that build a much smaller biofilm because they are not aciduric (don't make acid).
Pathogenic biofilm has a couple of requisites, and one is a low pH. So a biofilm with early colonizers that doesn't make acid has a harder time harboring the bacteria that we associate with dental disease. Harnessing this pH characteristic of biofilm goes right up into the face of traditional methods -- brush 'n' floss. Adjusting the pH allows your patients a way to manage their biofilm without having the dexterity and laser-focused education of a dental hygienist.
This pH alteration is energized by one particular friendly bacteria in the ProBiora3 family. Streptococcus oralis KJ3 and Streptococcus uberis KJ2 give off hydrogen peroxide. Take a shade guide picture before starting your patients on the Evora probiotic and see if you notice a difference. Are the teeth lighter?
In the early days of caries bacteria study, it was learned that Streptococcus mutans that were fed sucrose would excrete massive amounts of the sticky goo called glycomatrix, mucopolysaccharide, or slime, as well as other complex and unflattering terms. This goo of the biofilm protects the population in order to survive unmolested by such things as antibiotics, toothbrushes, and floss. Supplying the mouth with the ProBiora3 complex populates the niche previously inhabited by Streptococcus mutans faster than Strep. mutans can.
That's not the only way to manage the pH though. You probably already know that rinsing with a weak solution of hypochlorite (bleach), or a concoction of baking soda in water, or with xylitol will also raise the pH (see Figure 4). Only one of these options is yummy. A yummy factor must be part of any recommended protocol. The CariFree system harnessed the science with the good flavor into a mouth rinse and oral spray that alter the oral pH to favor healthy bacteria. Oragenics and CariFree may look at the synergy between the two products. Lower oral pH may accelerate the probiotic's effectiveness. Stay tuned.
The story of oral probiotics gets better! This way of biofilm management is not the wave of the future any longer. Recommending oral probiotics with natural strains from healthy mouths may be the ticket for patients who cannot or will not remove their own biofilm to dental hygienist standards.
Functional foods
Other fun ways to help patients manage their oral biofilm require dusting off your nutrition books. When you use the Nutritional Counseling Code, you have more to talk about than hidden sugar in a can of soda pop. Sugar supplies bacteria with the energy to produce the acids to dissolve enamel, or to initiate the inflammatory cascade associated with periodontal disease. Avoiding sugar and refined carbohydrates is a good goal, but nearly impossible for most mortals. Other dietary changes can interfere with the day-to-day function of ordinary biofilm, such as incorporating functional foods into the diet.
Using some sweeping generalities, it can be said that the best foods for biofilm management are licorice root, dark colorful berries, tea (black and green, iced or hot), cocoa, and coffee. These types of functional foods work directly on the biofilm as an entity. To be more specific, proanthocyanidins and resveratrol, which are types of flavonoids, are biofilm management tools.
Many of the foods containing these two flavonoids interfere with the biofilm's ability to adhere to the teeth, or with the early colonizer's ability to make the sticky matrix. These flavonoids also work by interfering with quorum sensing, which is the way the bacteria communicate with one another.
It would be a mistake not to mention the overall healthy benefits of foods high in flavonoids. Dr. Roizen of the Cleveland Clinic (www.sharecare.com/question/what-health-benefits-of-flavonoids) answers the question: What are the health benefits of flavonoids?
"Only about 16 choices in nutrition have been shown to make a difference in mortality rates, and consumption of flavonoids is one. Flavonoids decrease the rate of arterial and immune aging. These substances are like vitamins, but unlike vitamins are not essential for life. Flavonoids are powerful antioxidants, even more powerful than vitamins C and E combined. They also have anti-inflammatory effects that help keep our immune system young." Don't you just love it when something you recommend for oral health affects the rest of the body so positively?"
Xylitol fits into the functional foods category as well. It's seen by the bacteria as a food, so even if the gooey matrix is thick, xylitol makes it in and gums up the whole system in our favor. Bacteria cannot metabolize the five carbon structures and their metabolic system breaks down -- less acid, less goo, less visible plaque, and less invisible biofilm growing in the secret compartments between the papillae on the tongue and the mucosal cells on the cheeks and gingivae.
Due to requests by insurance companies, the Xlear company, maker of Spry products, offers a kit of xylitol products that lasts 30 days. XyliMelt by OraHealth is candy that adheres to the mucosa, and is effective for people who just want to have some candy melt in their mouths for a few hours. Similarly, Nuvora Inc. has products that adhere to the tissue and release xylitol and essential oils into the mouth for hours.
When giving brush 'n' floss directions, we end up focusing only on the teeth, and we miss the elephant in the room -- the tongue. Tongue coating is not innocuous, nor is it only a cosmetic concern. Biofilm on the tongue releases planktonic bacteria in what's called a planktonic storm. A coated tongue sends new biofilm to the rest of the mouth. A coated tongue even increases the chance of pneumonia in immunocompromised people.
In long-term care, this problem is called aspiration pneumonia and costs the government (read you and me) nearly $1 billion a year. Oraspa teaches a specific protocol for a tongue prophylaxis, so it's time for the tongue to be included in discussions about biofilm management. Xylitol, probiotics, and foods rich in flavonoids address all oral biofilm. (For more information about how scientists view the consequences of biofilm, go to www.tinyurl.com/shirleybiofilm.)
Prescriptions
Using these products and foods is simple. However, some of them will fit into your patients' routine better than others, so knowing how to recommend them is important.
According to Oragenics, their Pro version of oral probiotic should be used twice a day for the first 10 days after a professional prophylaxis, then once a day after that. For an in-depth view of oral probiotics, visit RDH eVillage (www.dentistryiq.com/articles/2012/05/gutkowski-probiotics.html).
Xylitol should be included in a Strive for Five arrangement. Five servings in any configuration a day, meaning gums, mints, toothpaste, oral spray, or any other way should be the goal.
Functional foods containing flavonoids should be used many times a day. Resist things such as cranberry extracts in tablet or capsule form. The food needs to be in contact with the structures of the mouth to exhibit a healthy effect.
Reexamination
Can you feel the neurogenesis in your brain? Now ask yourself -- if you cannot motivate someone to achieve total dental biofilm removal with a toothbrush, can you get them to drink coffee, hot cocoa, green or black tea, dark berry juices, or eat xylitol candy? Can you get them to incorporate one single probiotic tablet a day into their routine? Using these tools addresses the forgotten reality of how much room a biofilm needs, the complexity of a mature biofilm, and the size of human cells. Stop wearing the badge of "Floss Nag" with pride. Serve yourself and your patients better by offering scientifically proven oral health-promoting products.
SHIRLEY GUTKOWSKI, RDH, BSDH, FACE, is a clinical dental hygienist. Her experience and free thinking have made her a popular international speaker and award-winning author. She is the author of many books, chapters, and articles to support dental hygienists, and she is a career coach at CareerFusion. Her books can be purchased through www.rdhpurpleguide.com. Information on CareerFusion is at www.Careerfusion.net.
Past RDH Issues