A focus on periodontal maintenance
By Sue P. Humphrey, RDH, MSEd, FAADH, and Pinar Emecen Huja, DDS, PhD
Regenerative surgical procedures have long been regarded as an appropriate method for attempting to restore lost periodontal structure and functional attachment through the regeneration of cementum, periodontal ligament, and alveolar bone.1 Many studies point to the importance of plaque control and routine maintenance (supportive therapy) in the long-term success of sites treated with regenerative techniques.2 But the question of timing and the stages of care involved in plaque control and routine nonsurgical periodontal assessment and therapy after the surgical procedure can greatly affect the success of regenerative surgical care. The purpose of this article is to review the literature concerning the appropriate timing of procedures related to oral hygiene and supportive care of periodontal regeneration therapy. Also a timetable is presented as a practical guide for suggested nonsurgical care of patients receiving regenerative therapy.
--------------------------------------------------------------
See related articles
- Regeneration: a how-to for hygienists
- Guided tissue regeneration: background to current indications and applications
- Study finds that shorter waiting time between dental procedures is adequate
--------------------------------------------------------------
The goal of periodontal therapy is to establish a healthy periodontium and, if possible, restore lost form and function. Modes of healing in this endeavor can be characterized as either repair or regeneration.3 In repair, healing has occurred without sites returning to their original structural condition via a long junctional epithelial formation. This is the typical result of nonsurgical and conventional surgical therapies. Regeneration indicates that healing has occurred with restored architecture, including alveolar bone, cementum, and periodontal ligament. Such results occur with surgical treatment of defects with the use of bone grafting materials, guided tissue regeneration (GTR) procedures, or use of enamel matrix derivative (EMD).1,4
Wound healing
A very brief review of the general concepts of regenerative surgical considerations will guide the discussion of relative oral hygiene and supportive care as evidenced in current literature. Leading the discussion is a review of wound healing. Overall, wound healing principles of an intrabony defect are similar to the wound healing principles of an extraction site. Ideally, a clot fills the defect, containing blood factors necessary for normal wound healing. At the same time, the epithelium from the wound margins migrates slowly into the wound site over the clot. Early bone formation occurs as early as two months postoperatively and mature calcification is radiographically visible at six months.5
Healing during periodontal regeneration surgery differs somewhat from conventional periodontal surgical and nonsurgical outcomes. With conventional surgery and nonsurgical therapy, true regeneration (restoration of cementum, periodontal ligament, and alveolar bone) seems to be limited to the most apical portion of the defect. Healing occurs with the presence of long junctional epithelium along most of the root surface, even next to observed bone fill. This situation, while healthy, is functionally unconnected and only indirectly contributes to tooth stability. In contrast, as a result of successful regenerative periodontal surgery, new attachment apparatus forms in intrabony defects through differential tissue response, which increases functional periodontal support. This support occurs via increasing bone level, reducing crestal bone loss, increasing clinical attachment levels, and reducing pocket probing depths. Thus the use of regenerative periodontal procedures that include bone graft materials and membranes generally produce greater intrabony bone defect fill than flap debridement alone.6-7 Overall, regenerative periodontal procedures were found consistently more effective than open-flap debridement in the gain of clinical attachment and probing depth reduction in the treatment of intrabony and furcation defects.7-10
Regenerative grafting materials and techniques
Grafting material used during regenerative procedures may be autogenous (harvested from patients’ own bone) or allogenic bone (from another individual of the same species). Both of these materials can result in successful regeneration of the bone and its supporting apparatus, including cementum and periodontal ligament. Other types of grafting material may include alloplastic (synthetic bone substitutes) or xenografts (grafts taken from donors of another species). While alloplasts and xenografts function as biocompatible space fillers and result in little if any true regeneration, the use of these materials can stimulate bone growth and serve as a scaffold for new bone deposition.1 The resulting bone fill may also be accompanied by development of a long junctional epithelium and/or gain of connective tissue attachment.4
In addition to the choice of bone grafting materials, a decision must be made concerning the use of barriers in regenerative treatment. Barriers, whether resorbable or nonresorbable, can be used to exclude the in-growth of epithelium and connective tissue cells at the surgical site.1 Strict protocol to minimize membrane barrier contamination and infection correlates with clinical healing response.11 While the majority of studies in guided tissue regeneration report using nonresorbable barriers (which require a surgical site re-entry for retrieval), comparable favorable results have been shown from use of either type of membrane.4-5 GTR with barriers has also been successfully used in regenerating furcation defects, producing greater clinical improvements than GTR alone.12
Another surgical technique to attempt regenerating periodontal tissues is use of enamel matrix derivative (EMD). Emdogain is an FDA-approved, commercially available regeneration material, which is composed of enamel matrix proteins known as amelogenins.13 During tooth development, amelogenins are found to play a role in formation of tooth-supporting apparatus. Therefore, it is anticipated that use of EMD in periodontal defects would induce formation of periodontal attachment.14 Results from a human histologic study have suggested EMD can show evidence of periodontal regeneration on hopeless teeth.15 A recent systematic analysis on the efficacy of EMD in regenerative procedures concluded that in treatment of intrabony defects, EMD is superior to open-flap debridement and as effective as resorbable membranes.16 Regenerative therapies performed either with GTR or EMD were proved to achieve predictable clinical success by clinical attachment level gain and tooth maintenance.17-18 (see Figure 1)
Factors affecting regeneration outcomes
Long-term stability of positive clinical outcomes of regenerative procedures were found to be dependent upon patient and defect-related variables such as smoking status or participation in periodontal maintenance programs or radiographic angle of the defect. However, it has been indicated that if periodontal regenerative therapy is guided by literature support and proper case selection, the long-term stability was mostly dependent on patient-related variables.18 Such patient-related variables for the long-term stability of regenerated sites include plaque control and recall compliance. Failure of the patient to maintain high levels of plaque control and regular periodontal recalls can result in disease reoccurrence with suspected periodontal pathogens at a four times greater rate.19 Other factors that may affect the successful outcome of periodontal regenerative surgery include systemic conditions such as uncontrolled diabetes. Surgical considerations such as infection control, defect morphology, surgical technique, and wound stability can also influence healing response.2,4,20
Typical healing patterns in GTR surgery, representing about three-quarters of treated patients with good compliance, plaque control, and postoperative care, exhibit the following timetable of healing: granulation tissue at six to eights weeks, keratinization of exposed new tissue at eight to 12 weeks, and bone fill at three to 12 months, with favorable maturation of all tissues at six months.21 The presence of pathogenic flora impacts the success of regenerative procedures before, during, and after the actual surgical procedure.11 High bacterial counts and the persistence of specific pathogens in the pocket before surgical treatment, especially A.a. in the intrabony defect, are negatively associated with the outcome of treatment.22
Periodontal maintenance following regenerative procedures
Oral hygiene instructions should be given and subsequently evaluated, resulting in lower plaque scores (reported from different sources <15% to <25%), to determine patient compliance before the surgical procedure. The patient must understand his or her role in contributing to the successful outcome of the surgery. Initial scaling and root planing is performed, dependent upon the patient’s oral hygiene and presence of bacterial deposits.5,23 As to the optimal timing of the anti-infective therapy and mechanical debridement before surgery, no discernible difference has been found between patients who receive the therapy before surgery as part of the hygienic phase and those who receive the therapy at the time of surgery. The point is that the anti-infective therapy be performed and that the patient remain on a strict oral hygiene regimen with absence of inflammation during the healing stage for optimal results.24
Other anti-infective modalities used to eliminate or reduce pathogens prior to regenerative surgery may include treatment of periodontal lesions other than those designated for regenerative therapy. Patients who received pocket reduction therapy prior to regenerative surgery exhibited low levels of barrier membrane contamination and the most clinical attachment gain.23 Nondental ecological niches for periodontal pathogens within the oral cavity are generally not affected by mechanical debridement and serve as sources of intraoral transmission. Also, postoperative antibiotic use is empiric with the rationale for use being suppression of subgingival plaque formation rather than only as a preventive of postoperative infections.25 Use of substantive antimicrobials such as .12% chlorhexidine is also indicated for a period of time postoperatively.22
Regenerated tissue should be protected during the maturation phase. The patient should be advised to avoid disturbing the surgical site for a short period of time immediately following surgery. Gentle wiping or brushing of the site may begin within several days of the procedure, based on the surgeon’s recommendation. References vary on the subject of postoperative tooth brushing at the surgical site, from waiting until after the first postoperative visit to waiting for six weeks.17,19,20 If a nonresorbing barrier is used, no flossing should be performed before removal of the barrier.26
As to professional postoperative care, only supragingival prophylaxis of the area is recommended until the site is evaluated by the surgeon and found to be ready for subgingival introduction of assessment and debridement instruments.22 Frequent professional plaque removal during the healing period is advised. Supportive supragingival periodontal therapy treatment may be used once a week for six weeks following the surgery and then one time per month for six months.27 Subgingival probing and scaling and the use of pumice are to be avoided for a six-month period to allow maturing of newly formed connective tissue.28
The optimum periodontal supportive therapy after regenerative procedures has not been firmly established. It should be based on individual need and follow general anti-infective guidelines for conventional maintenance therapy with a few considerations.29 It has been found that proper oral hygiene resulting in decreased plaque levels results in more successful regenerative procedure results than that of patients with higher plaque levels.30 Additionally, patients with good oral hygiene preserve the clinical attachment gain achieved through regenerative procedures for many years.31
The clinical methods used to evaluate therapeutic endpoints of regenerative surgery at the six-month postsurgical timeframe include various assessments of gingival inflammation, periodontal probing, radiographs, and re-entry procedures. Results are determined by comparing pre- and posttreatment measurements.4 Periodontal probing is the most frequently used examination to assess the clinical effect of regenerative procedures in a practice setting.32
Long-term success (three or more years) following GTR procedures in intrabony defects is directly related to compliance with maintenance visits and plaque-control procedures. Because the success of regenerative procedures is dependent on proper postoperative care, the patient must be willing and able to keep follow-up visits. The results of noncompliance have been disappointing.25 It has been shown that sites receiving only sporadic care lost previously gained clinical attachment with GTR pretreatment levels. The presence of plaque, bleeding on probing, and/or P. gingivalis were significant markers of attachment loss.17,19
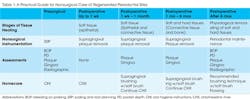
The successful treatment of periodontal defects with regenerative surgical modalities is greatly impacted by the control of plaque bacteria and carefully timed nonsurgical supportive care. All members of the dental team delivering care to the patient surrounding the regenerative surgical procedure should be in communication with the surgeon and the general dentist in order to plan the best anti-infective care for the patient. Understanding the necessity of strict plaque control coupled with the knowledge of the varying stages of healing of the different tissues in the surgical site will allow for the most optimum treatment outcome (see Table 1).
Sue P Humphrey, RDH, MSEd, FAADH, and Pinar Emecen Huja, DDS, PhD, teach in the division of periodontology at University of Kentucky College of Dentistry. Humphrey can be contacted at [email protected].
References
1. AAP. "Position Paper on Periodontal Regeneration." J Periodontal Sept. 2005;76(9):1601-1622.
2. Cortellini P, Bowers G. Periodontal regeneration of intrabony defects: an evidence-based treatment approach. Int J Periodont Rest Dent 1995;15(2):129-145Becker,
3. Caton J, Greenstein G. Factors related to periodontal regeneration. Periodontal 2000 1993;1:9-15.
4. Garrett S. Periodontal regeneration around natural teeth. Annals of Periodontology 1996;1:621-666.
5. Becker W, Becker B. Periodontal regeneration: a contemporary re-evaluation. Periodontal 2000 1999;19:104-114.
6. Reynolds M, Aichelmann-Reidy M, et al. The efficacy of bone replacement grafts in the treatment of periodontal osseous defects. A systematic review. Ann Periodontal 2003;8:227-265.
7. Sculean A, Nikolidakis D, Schwarz F. Regeneration of periodontal tissues: combinations of barrier membranes and grafting materials — biological foundation and preclinical evidence. A systematic review. J Clin Periodontol. 2008;35(suppl 8):106-116.
8. Murphy K, Gunsolley J. Guided tissue regeneration for the treatment of periodontal intrabony and furcation defects. A systematic review. Annals of Periodontology 2003;8(1):266-302.
9. Needleman I, Worthington HV, Giedrys-Leeper R, Tucker R. Guided tissue regeneration for periodontal infra-bony defects. A review. Cochrane Database of Systematic Reviews. 2006; issue 2.coc.
10. Venezia E, Goldstein M, Boyan BD, Schwartz Z. The use of enamel matrix derivative in the treatment of periodontal defect: a literature review and meta-analysis Crit Rev Oral Biol Med. 2004;15:382-402.
11. Nowzari H, Matian F, et al. Periodontal pathogens on polytetrafluoroethylene membrane for guided tissue regeneration inhibit healing. J Clin Perio 1995;22:469-474.
12. Evans G, Yukna R, et al. Frequency of furcation closures with regenerative periodontal therapy. J West Soc Periodontal Periodontal Abstract 1996;44:101-109.
13. Hammarström L. Enamel matrix, cementum development and regeneration. J Clin Periodontol 1997;24:658-668.
14. Esposito M, Grusovin MG, Papanikolaou N, Coulthard P, Worthington HV. Enamel matrix derivative (Emdogain®) for periodontal tissue regeneration in intrabony defects. A Cochrane systematic review. Eur J Implantol. 2009;2:427-266.
15. Yukna RA, Melloning JT. Histologic evaluation of periodontal healing in humans following regenerative therapy with enamel matrix derivative. A 10-case series. J Periodontal 2000;71:752-759.
16. Koop R, Merheb J, Quiryen M. Periodontal regeneration with enamel matrix derivative in reconstructive periodontal therapy: A systematic review. J Periodontol 2012;707-720.
17. Cortellini P, Tonetti MS. Long-term tooth survival following regenerative treatment of intrabony defects. J Periodontol 2004;75:672-678.
18. Silvestri M, Rasperini G, Milani S. 120 infrabony defects treated with regenerative therapy: long-term results J Periodontol 2011;82:668-675.
19. Cortellini P, Prato GP, et al. Periodontal regeneration of human infrabony defects (v). Effect of oral hygiene on long-term stability. J Clin Periodont 1994;21:606-610.
20. Trombelli L, Kim C, et al. Retrospective analysis of factors related to clinical outcome of guided tissue regeneration procedures in intrabony defects. J Clin Perio 1997;24: 366-371.
21. Schallhorn R, McClain P. Clinical and radiographic healing pattern observation with combined regenerative techniques. Int J Periodontol Rest Dent 1994;14(5):391-403.
22. Heitz-Mayfield L, Tonetti M, et al. Microbial colonization patterns predict the outcomes of surgical treatment of intrabony defects. J Clin Perio 2006;33:62-68.
23. Way H, MacNeil R. Guided tissue regeneration: Absorbable Barriers. Dental Clinics of North America 1998;42(3):505-521.
24. Machtei E, Cho M, et al. Clinical, microbiological and histological factors which influence the success of regenerative periodontal therapy. J Periodontol 1994;65:154-161.
25. Gray J, Hancock E. Guided tissue regeneration: nonresorbable barriers. Dental Clinics of North America 1998;42(3):523-541.
26. Tonetti M, Pini-Prato G, et al. Periodontal regeneration of human intrabony defects IV. Determinants of healing response. J Periodontol 1993;64:934-940.
27. Nowzari H, Macdonald ES, et al. The dynamics of microbial colonization of barrier membrane for guided tissue regeneration. J Periodontol 1996;67:694-702.
28. Slots J, MacDonald EM, et al. Infectious aspects of periodontal regeneration. Periodontol 2000 1999;19:164-172.
29. Wilson TG. Supportive periodontal treatment and re-treatment in periodontics. Periodontol 2000 1996;12:7-140.
30. Tonetti M, Prato GP, et al. Factors affecting the healing response of intrabony defects following guided tissue regeneration and access flap surgery. J Clin Perio 1996;23:548-556.
31. Cortellini P, Prato, GP, et al. Long-term stability of clinical attachment following guided tissue regeneration and conventional therapy. J Clin Perio 1996;23:106-111.
32. Reddy MS, Jeffcoat MK. Methods of assessing periodontal regeneration. Periodontal 2000. 1999;19:87-103.
Past RDH Issues