Can you hear me now? Occupational noise-induced hearing loss among dental professionals
For the past 25 years, dental professionals have become increasingly aware of the number of occupational hazards associated with working in a dental office. We protect our skin with gloves and lab jackets, our eyes with protective eyewear, our noses and mouths with masks and face shields, and our neck, shoulder, and back postures with loupes and saddle stools. But what about our ears? To date, most dental health-care workers have not taken an active role in protecting their hearing in the workplace.
Noise is everywhere. When it comes to noise, the dental office is a polluted environment. Dental heath-care workers are constantly subjected to both intermittent and continuous noise from high-speed handpieces, ultrasonic scalers, suction devices, automated mixers, ultrasonic instrument cleaners, instrument dishwashers, vacuum pumps, air compressors, model trimmers, business office equipment, telephones, entertainment systems, and heating and air-conditioning units.
Due to infection control concerns, today's dental offices are designed with hard surfaces that are easy to clean. But instead of absorbing sound well, hard surfaces radiate sounds throughout the office. Along with the design changes found in dental offices, today's trend is to build larger and larger multitreatment-room group practices that provide care from dawn to well into the evening hours, often open six days a week or even more. We spend our days immersed in a big vat of never-ending sound.
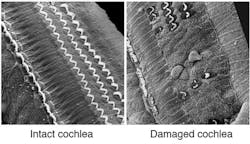
Both hearing loss and tooth loss were once considered a natural part of aging. Just as natural tooth surfaces can reach a point where the damage to the hard surfaces can't be reversed, damage to our auditory apparatus can be permanent as well. The cochlea is the inner ear structure responsible for hearing acuity. It contains a finite number of structures called hair cells, which are responsible for sending hearing messages via the auditory nerves to the brain. In direct response to excessive noise levels, hair cells can become damaged over time and eventually die. At this point, there are no methods to repair damage to the inner and outer hair cells in the cochlea.
Just as it is important to preserve tooth structure, dental professionals need to protect their hearing.
Types of hearing impairment
Sensorineural hearing loss (SNHL) is the most common type of hearing loss and occurs when there is damage to the cochlea or to the nerve pathways from the inner ear to the brain. SNHL reduces the ability to hear faint sounds. Even if speech is loud enough, it can be muffled or unclear, setting the stage for significant communication problems. While there are other suspected causes for SNHL, noise remains the largest factor in the development of this type of hearing disability. Other contributing factors include illness, certain drugs, genetic predisposition, aging, head trauma, and inner ear malformations.1,2
Loud noise exposure can also cause tinnitus, which is classified as a hearing impairment but not a true hearing loss. Most who suffer from tinnitus complain of ringing, buzzing, roaring, or hissing sounds when there is not an actual noise source to create this sensation. Tinnitus may subside over time or can continue constantly or occasionally throughout a person's life.3 Tinnitus is more common for those with hearing difficulties. The risk for developing both tinnitus and hearing loss rises with the number of years on a noisy job.4
Temporary hearing loss that disappears within 16 to 48 hours can also be a result of exposure to continuous loud noise or a loud impulse. Even though the temporary hearing loss may seem to go away, there may be long-term damage.
Prevalence and symptoms
Hearing problems are a classic outcome of aging. Twenty-five percent of Americans between ages 65 and 74 report hearing issues, and 50% over the age of 75. But concluding that age is the real culprit does not take into account that approximately 26 million Americans, or one in ten between ages 20 and 69 have high-frequency hearing loss from overexposure to loud noise at work or during leisure activities.1 Twenty-three percent of those exposed to occupational noise report hearing difficulty, 15% had tinnitus, and 9% had both conditions, findings that are significantly higher than workers who are not exposed to noise.5
Data analysis from the 2005-2006 NHANES study reported one in five U.S. adolescents demonstrated hearing loss. While the hearing loss of most adolescents was classified as slight, the prevalence had increased over the previous nine-year period of time.6 Sixteen percent of teens, ages 12 to 19, report some hearing loss, thought to be caused by exposure to loud noise.1 Sixty-six percent of college students in a single study reported experiencing tinnitus.7 More than 30 million Americans of all ages are exposed to dangerous levels of noise on a regular basis.
Over time, the sounds a person hears become muffled or distorted. A classic symptom of NIHL is difficulty in understanding everyday conversations. Other indicators of a hearing problem include:
- Trouble hearing a phone conversation
- Difficulty in following a conversation with two or more people or straining to hear what is being said
- Trouble hearing when there is background noise
- Asking people to repeat themselves
- Thinking people are mumbling or not speaking clearly
- Misunderstanding what others are saying, or turning up the radio or TV volume too high
Symptoms of NIHL increase gradually over time, and the person may not be aware of the loss, which can be confirmed with a hearing test. Noise-induced hearing loss is cumulative, invisible, and permanent.8
Impact on daily living
Hearing impairment at all levels compromises communication, can play a role in workplace safety, result in social isolation, lead to depression, and higher rates of mental and physical illness.9 The direct and indirect costs to society continue to mount as more people develop compromised hearing.
Men are twice as likely than women to experience severe hearing loss. Tinnitus and hearing difficulties increase as the number of years working in a noisy environment rises.4 Current and former smokers are at increased risk for hearing difficulty throughout their lifetime.10
Noise exposure can lead to annoyance, sleep disturbances resulting in daytime sleepiness, impaired cognitive performance, fatigue, and an increased risk for hypertension and cardiovascular disease.11 A recent study showed exposure to daytime noise can cause heart rate variability.12
Hearing depends on a complex series of events in the human ear. Soundwaves in the air travel from the outer ear through the middle ear to the cochlea in the inner ear. The cochlea is lined with between 17,500 and 23,500 inner and outer hair cells. Individual hair cells are responsible for very specific auditory frequencies. Tiny projections on the top of the hair cells are called stereocilia. As the soundwaves reach the inner ear, healthy hair cells move back and forth rhythmically in the fluid-filled cochlea. The outer hair cells amplify the sounds and the inner hair cells create electrical signals. These signals are carried by the auditory nerve to the brain, which translates signals into recognizable sounds. Most NIHL involves damage to cochlear hair cells.3
Each individual's personal hair cell count is determined long before we ever hear our first sound. The total number of hair cells an individual human receives is determined around 10 weeks of fetal gestation.13 Repeated or long exposures to sounds above 85 bB, or sudden loud bursts above this critical decibel level, can wreak havoc on hair cells and their response to soundwaves. Exposure to undue noise stress causes delicate hair cells to begin to collapse or break, making it impossible to process certain sounds. Unlike other body tissues, damaged or dead hair cells cannot be repaired or regenerated.3
Noise levels
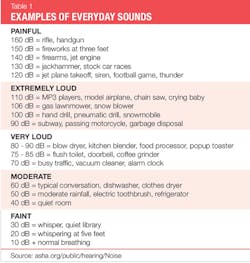
Every sound has a specific pitch or frequency and its own loudness or intensity. Hearing tests assess the ability to hear specific sound frequencies from low to high pitches. Frequencies are measured in hertz (Hz). The human auditory system can hear a wide range of frequencies from 125 Hz to 8,000 Hz. Frequency levels between 2,000 Hz and 8,000 Hz are considered high frequency. The loudness or intensity of a sound is measured in decibels. The decibel scale begins at zero, which is near total silence. Decibels are measured in a logarithmic scale.14
A normal conversation at 60 decibels is significantly more intense than a whisper at 30 dB and sounds twice as loud. Repeated exposure to sounds at or above 85 dB over time can cause permanent hearing loss. Noise levels at 140 dBa can cause hearing damage with just one exposure. An "A-weighted" decibel, reported as a dBa, is designed to mimic the response of the human ear.14
The length of time one is exposed to dangerous sound levels is also important-the longer the exposure time, the greater the risk. In addition, the louder the sound, the shorter the exposure time before damage occurs. According to the National Institute for Occupational Safety and Health (NIOSH), the maximum exposure time at 85 dB is eight hours. In contrast, the maximum exposure time at 110 dB, is one minute and 29 seconds. A three dB increase alone doubles the amount of noise, and halves the recommended amount of exposure time.
Basic hearing hygiene recommends avoiding noises that are too loud, too nearby, or last too long-a nearly impossible set of recommendations for those working in a dental office.15 The noise meter on the NIOSH site demonstrates decibel levels versus time exposures by using common sounds. For example, a power lawnmower operates at 90 dB, a noise level only slightly above that of many ultrasonic dental scalers. To put this into perspective, NIOSH recommends no more than two hours of exposure to 90 dB on a daily basis.16
Additional life factors
Continuous noise is a part of modern life.17 Social noise exposure has tripled over the last three decades.2,7 Every household is filled with multiple noise sources from kitchen appliances to personal care products such as hair dryers, or entertainment systems or personal music devices.18,19
Televisions, electronic devices, video games, and computers add to the burden. Commuting typically involves additional noise exposure from traffic, sirens, buses, subway systems, and car stereos.17 Recreational activities such as power boating, car racing, riding off-road vehicles, and shooting firearms also contribute. Attending concerts, stadium-based sporting events, playing musical instruments,20,21,22 noisy classrooms, restaurants,23 and loud toys all play a role in modern-day noise pollution (see Table 1).
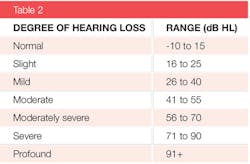
Audiologists perform a variety of tests for auditory acuity that document the ability to hear various levels of loudness (dB) and pitch ( measured in Hz). The hearing threshold is the sound level below which a human ear is unable to detect any sound. Zero dB is the adult reference level. As hearing becomes compromised, the lower limit rises; creating a temporary or permanent threshold shift that makes it difficult to hear soft sounds. Severity ranges from slight to profound and is based on a person's hearing loss range in decibels (dBHL) (see Table 2). As hearing loss progresses, it becomes more difficult to hear higher pitch noises, such as women's voices.14
Occupational hearing loss prevention
Workers exposed to excessive levels of noise can be found in all types of occupations. Workers at risk include textile workers, construction, farming, plumbing, firefighters, police, musicians, demolition, landscape workers, manufacturing, helicopter and plane pilots, and military. Many more occupations could be added to this list.
Two different federal agencies take an active role in workplace hearing loss issues. While the two agency goals are focused on hearing loss issues, their goals and scope are not the same. The Occupational Safety and Health Administration (OSHA) is a federal agency that regulates safety in the workplace. OSHA has established regulations for hearing protection and conservation. The National Institute for Occupational Safety and Health (NIOSH) is a federal research agency that makes recommendations and provides additional resources for preventing occupational hearing loss. OSHA has the power of law behind its regulations, while NIOSH's recommendations are not subject to workplace enforcement rules. NIOSH advises, but in the end does not have the enforcement power to protect workers.
It is interesting to note that NIOSH recommendations for decibel levels and time exposure are significantly more stringent than those posed by OSHA.24 A 2000 report speculated if OSHA were to adopt NIOSH's stricter noise exposure guidelines, the number of workers enrolled in a hearing loss prevention program would nearly triple.25
Countless papers have discussed dental office noise, as well as factors that may contribute to NIHL among dental professionals. Some research regarding noise in the dental setting has been conducted in dental school settings. It is hard to imagine that school settings are a mirror image to the amount of time one is exposed to noise in a busy dental office.26-28 Numerous studies express concern over the continuous, intermittent exposure of dental professionals to decibel levels that are consistent with known damage to the human auditory apparatus.26-34
The first high-speed air turbine handpieces were introduced over 50 years ago. Ten years later, the first ultrasonic dental scaler came on the market.29 Both devices gained wide acceptance and are routinely used worldwide. While the dB levels are based on the specific equipment tested,26-33 it is reasonable to consider that decibel level exposures fall somewhere in the reported ranges. A few studies compared new high-speed and ultrasonic scalers to used equipment (see Table 3). Used equipment produced higher decibel levels. Intensity levels for suction devices and slow-speed handpieces have also been evaluated.
Recent studies have shown that dentists who use high-speed handpieces have significant hearing loss as compared to dental students,35 other academic professionals,36 or physicians of the same age and length of practice.37 Hearing loss has been found in dentists who have practiced 10 or more years,37,38 and those over the age of 40.36,38 Both male and female dentists in the same age range develop hearing impairment.36,39
Hearing loss begins in the frequencies of 3, 4, and 6 kHz, eventually progressing to other ranges. Three to 6 kHz is the spectrum where a person loses the ability to hear high-pitched sounds.36,40 Hearing impairment among dentists is being reported at these frequencies.36,39,41 In addition, hearing thresholds are high for dentists.36,41
Only two studies specifically evaluated hearing loss issues among dental hygienists. The hearing status of hygienists who had a high rate of ultrasonic scaler usage was compared to hygienists who reported minimal use of these devices. Testing was conducted using a pure tone audiometer. There were no differences between the two groups in hearing threshold levels, but the high-usage group had hearing loss at 3 kHz. While the findings are an important start in understanding hearing loss among dental hygienists, the study did not control for type or condition of ultrasonic unit, power level control, or size, configuration, or diameter of the ultrasonic tip.42
In a self-administered questionnaire, 40% of respondents with an average age of 56 reported hearing difficulty. Respondents with hearing difficulty were twice as likely to report high use of ultrasonic scalers. Over 90% of those who reported hearing difficulty related to power scaler usage had their hearing loss confirmed by an audiologist.43 While there may be a strong correlation between ultrasonic usage and hearing impairment, this study also does not demonstrate causality.
Preventing NIHL
The first 10 years of excessive noise exposure are the most risky for developing NIHL. Since loss is cumulative, reducing the risk is critical at any career point, especially since high-frequency tones are most important to understanding speech.44 A standard audiogram provides a conventional hearing threshold evaluation. Since dental professionals are at increased risk for high-frequency hearing loss, additional tests such as high-frequency threshold audiometry can help in the early detection of NIHL.41
The web-based program, "It's a noisy planet: Protect their hearing," from National Institutes of Health focuses on protecting the hearing of children and adolescents but also contains a wealth of practical advice that is applicable to everyone. Before exploring our unique dental needs, here are the universal precautions recommended by the National Institute on Deafness and Other Communication Disorders.3
- Know which noises can cause damage (greater than 85 decibels).
- Wear earplugs or other protective devices.
- If you can't reduce noise, move away from it.
- Be alert to hazardous environmental noises.
- Protect the ears of children.
- Make family, friends, and colleagues aware of hazardous noise.
- Suspect hearing impairment? Get tested.
Since noise will always be a part of the dental environment, the most logical way to reduce the hazards of NIHL is to work with equipment that is less noisy and to use some form of direct hearing protection.44,45 Handpieces are now made that are much quieter than earlier models. Poorly maintained or worn-out high-speed handpieces are noisier. Daily maintenance will keep equipment running smoother and prevent handpieces from wearing out prematurely.37 Quiet compressors are now available. Portable and mobile dental units are now made with quieter components.
The other strategy is to use adequate ear protection every day, all day long.44,45 Very few clinicians receive training about hearing protection during school, so many are not aware of their hearing protection options, and some assume the noise is not damaging. Comfort, convenience, and efficacy play a huge role in implementing a hearing protection plan.
Cotton stuffed into the ear canal reduces sound by 7 dB and is not an effective protective device.46 Earplugs create a physical barrier when inserted correctly into the ear canal. However, while effective in reducing damaging noise levels, human speech is muffled and soft.
The three types of over-the-counter earplugs are foam, molded polyurethane, and silicone. Foam earplugs are single-use devices. The user needs to roll the plug in the palm of the hand to reduce the diameter and then insert the device into the ear canal. The compressed foam expands to create a seal. Molded polyurethane and silicone earplugs can be used more than once and can be cleaned between uses. None of these devices is designed for a custom fit, so it is important to take care in the installation process.
Earplugs are typically rated for noise reduction. An NR 25 has the capacity to reduce the decibel levels by 25, while one rated at NR 33 will have a greater capacity to reduce damaging noise levels.
Custom-made earplugs can be obtained from an audiologist. Impressions are taken for each ear, using materials similar to a dental impression. While these earplugs offer a custom fit, again, they are only designed to reduce noise input. Musicians' earplugs are designed with small filters that dampen down certain sound ranges while amplifying others. So these are not an ideal product for those of us in dentistry.
A new earplug called the DI-15 was introduced recently that is specifically designed for use by dental health-care workers. [Editor's note: Since the original publication date of this article, the DI-15 has been rebranded as EarAIDi]. The DI-15 is a "smart" ear protection technology fabricated with a custom electronic circuitry that compresses sound when the decibel levels reach the dangerous point. The noise reduction rating for the DI-15 is 25. The compression stops when noise levels fall back into a safer range.
In addition to compressing noise levels as needed, dental professionals can carry on a normal conversation with patients and other staff members. These earplugs are quite small and powered by a tiny hearing-aid battery that typically lasts approximately two weeks.
The DI-15 ear protector device is quite small and fits discreetly into the ear canal. The DI-15 ear protectors come with a series of six different types of silicone and memory foam plug-end adaptors, which allows the user to select the plug with the best fit to their own ears. It is also possible to attach custom-molded earplugs to the DI-15, providing the ultimate in personal customization. The plugs can be attached to a very thin, clear but sturdy lanyard that can hang around the neck when the plugs are not in the ears. The DI-15 ear protectors come with a small storage case.
Additional information for this novel protection device is available at dentalinnovationsllc.net. The company also offers the DI 20 patient noise protection earplugs that use disposable ear tips.
NIHL is permanent and preventable. Everyone in dentistry faces a much higher risk for developing hearing impairment. Dental professionals need to adopt a realistic, informed strategy to stop this needless epidemic. As one of my dental colleagues used to say, "There is no dentistry like no dentistry," we need to start thinking that "There is no hearing loss like no hearing loss."
Note
i. Update 11/7/2019: The DI-15 has been rebranded as EarAID and is manufactured by Forward Science.
References
1. It's a noisy planet. http://www.noisyplanet.nidcd.nih.gov/press/Pages/nihlfacts.aspx
2. Sliwinska-Kowalska M, Davis A. Noise induced hearing loss. Noise Health. 2012 Nov-Dec;14(61):274-80.
3. Noise-induced hearing loss. https://www.nidcd.nih.gov/health/noise-induced-hearing-loss
4. Palmer KT, Griffin MJ, Syddall HE, Davis A, Pannett B, Coggon D. Occupational exposure to noise and the attributable burden of hearing difficulties in Great Britain. Occup Environ Med. 2002 Sep;59(9):634-9.
5. Masterson EA, Themann CL, Luckhaupt SE, Li J, Calvert GM. Hearing difficulty and tinnitus among U.S. workers and non-workers in 2007. Am J Ind Med. 2016 Apr;59(4):290-300.
6. Shargorodsky J, Curhan SG, Curhan GC, Eavey R. Change in prevalence of hearing loss in US adolescents. JAMA. 2010;304(7):772-778.
7. Rawool VW, Colligon-Wayne LA. Auditory lifestyles and beliefs related to hearing loss among college students in the USA. Noise Health. 2008 Jan-Mar;10(38):1-10.
8. Hearing loss and older adults https://www.nidcd.nih.gov/health/hearing-loss-older-adults
9. Hearing loss in older adults tied to more hospitalizations and poorer physical and mental health. http://www.hopkinsmedicine.org/news/media/releases/. June 11, 2013.
10. Palmer K, Griffin M, Syddall H , Coggon D. Cigarette smoking, occupational exposure to noise, and self reported hearing difficulties. Occup Environ Med. 2004 Apr; 61(4): 340-344.
11. Basner M, Babisch W, Davis A, et al. Auditory and non-auditory effects of noise on health. Lancet. 2014;383(9925):1325-1332.
12. Kraus U, Schneider A, Breitner S, et al. Individual daytime noise exposure during routine activities and heart rate variability in adults: A repeated measures study. Environmental Health Perspectives. 2013;121(5):607-612.
13. Hair cells: overview. http://www.cochlea.eu/en/hair-cells
14. Noise. http://www.asha.org/public/hearing/Noise/
15. Noise and hearing loss prevention. http://www.cdc.gov/niosh/topics/noise/stats.html
16. Noise and hearing loss prevention. Noise meter. phttp://www.cdc.gov/niosh/topics/noise/noisemeter.html
17. Kraus U, Breitner S, Hampel R, Wolf K, Cyrys J, Geruschkat U, Gu J, Radon K, Peters A, Schneider A. Individual daytime noise exposure in different microenvironments. Environ Res. 2015 Jul;140:479-87.
18. Jiang W, Zhao F, Guderley N, Manchaiah V. Daily music exposure dose and hearing problems using personal listening devices in adolescents and young adults: A systematic review. Int J Audiol. 2016 Jan 15:1-9.
19. Muchnik C, Amir N, Shabtai E, Kaplan-Neeman R. Preferred listening levels of personal listening devices in young teenagers: self reports and physical measurements. Int J Au-diol. 2012 Apr;51(4):287-93.
20. McIlvaine D, Stewart M, Anderson R. Noise exposure levels for musicians during rehearsal and performance times. Med Probl Perform Art. 2012 Mar;27(1):31-6.
21. Gopal KV, Chesky K, Beschoner EA, Nelson PD, Stewart BJ. Auditory risk assessment of college music students in jazz band-based instructional activity. Noise Health. 2013 Jul-Aug;15(65):246-52.
22. Dudarewicz A, Pawlaczyk-Łuszczynska M, Zamojska-Daniszewska M, Zaborowski K. Exposure to excessive sounds during orchestra rehearsals and temporary hearing changes in hearing among musicians. Med Pr. 2015;66(4):479-86.
23. Lao XQ, Yu IT, Au DK, Chiu YL, Wong CC, Wong TW. Noise exposure and hearing impairment among Chinese restaurant workers and entertainment employees in Hong Kong. PLoS One. 2013 Aug 15;8(8):e70674.
24. Neitzel R. NIOSH and OSHA permissible noise exposure limits http://www.audiologyonline.com/ask-the-experts/niosh-and-osha-permissible-noise-247.
25. Sriwattanatamma P, Breysse P. Comparison of NIOSH noise criteria and OSHA hearing conservation criteria. Am J Ind Med. 2000 Apr;37(4):334-8.
26. Qsaibati ML, Ibrahim O. Noise levels of dental equipment used in dental college of Damascus University. Dent Res J (Isfahan). 2014 Nov;11(6):624-30.
27. Dutta A, Mala K, Acharya SR. Sound levels in conservative dentistry and endodontics clinic. J Conserv Dent. 2013 Mar;16(2):121-5.
28. Kadanakuppe S, Bhat PK, Jyothi C, Ramegowda C. Assessment of noise levels of the equipments used in the dental teaching institution, Bangalore. Indian J Dent Res. 2011 May-Jun;22(3):424-31.
29. Altinöz HC, Gökbudak R, Bayraktar A, Belli S. A pilot study of measurement of the frequency of sounds emitted by high-speed dental air turbines. J Oral Sci. 2001 Sep;43(3):189-92.
30. Bali N, Acharya S, Anup N. An assessment of the effect of sound produced in a dental clinic on the hearing of dentists. Oral Health Prev Dent. 2007;5(3):187-91.
31. Sorainen E, Rytkönen E. Noise level and ultrasound spectra during burring. Clin Oral Investig. 2002 Sep;6(3):133-6.
32. Yousuf A, Ganta S, Nagaraj A, Pareek S, Atri M, Singh K, Sidiq M. Acoustic noise levels of dental equipment and its association with fear and annoyance levels among patients attending different dental clinic setups in Jaipur, India. J Clin Diagn Res. 2014 Apr;8(4):ZC29-34.
33. Sorainen E, Rytkönen E. High-frequency noise in dentistry. AIHA J (Fairfax, Va). 2002 Mar-Apr;63(2):231-3.
34. Saini R, Saini G, Saini S; Sugandha. Dental practice and perilous auditory effect as occupational hazard. Noise Health. 2010 Jan-Mar;12(46):56.
35. Theodoroff SM, Folmer RL. Hearing loss associated with long-term exposure to high-speed dental handpieces. Gen Dent. 2015 May-Jun;63(3):71-6.
36. Willershausen B, Callaway A, Wolf TG, Ehlers V, Scholz L, Wolf D, Letzel S. Hearing assessment in dental practitioners and other academic professionals from an urban setting. Head Face Med. 2014 Jan 18;10:1.
37. Messano GA, Petti S. General dental practitioners and hearing impairment. J Dent. 2012 Oct;40(10):821-8.
38. Khaimook W, Suksamae P, Choosong T, Chayarpham S, Tantisarasart R. The prevalence of noise-induced occupational hearing loss in dentistry personnel. Workplace Health Saf. 2014 Sep;62(9):357-60.
39. Gurbuz MK, Çatli T, Cingi C, Yaz A, Bal C. Occupational safety threats among dental personnel and related risk factors. J Craniofac Surg. 2013 Nov;24(6):e599-602.
40. Metidieri MM, Rodrigues HF, Filho FJ, Ferraz DP, Neto AF, Torres S. Noise-induced hearing loss (NIHL): Literature review with a focus on occupational medicine. Int Arch Otorhinolaryngol. 2013 Apr;17(2):208-12.
41. Lopes AC, de Melo AD, Santos CC. A study of the high-frequency hearing thresholds of dentistry professionals. Int Arch Otorhinolaryngol. 2012 Apr;16(2):226-31.
42. Wilson JD, Darby ML, Tolle SL, Sever JC Jr. Effects of occupational ultrasonic noise exposure on hearing of dental hygienists: a pilot study. J Dent Hyg. 2002 Fall;76(4):262-9.
43. Lazar A, Kauer R, Rowe D. Hearing difficulties among experienced dental hygienists: A survey. J Dent Hyg. 2015 Dec;89(6):378-83.
44. Occupationally induced hearing loss. DHHS (NIOSH) Publication No. 2010-136. http://www.cdc.gov/niosh/docs/2010-136/pdfs/2010-136.pdf
45. Lusk SL. Noise exposures. Effects on hearing and prevention of noise induced hearing loss. AAOHN J. 1997 Aug;45(8):397-408.
46. A call for hearing protection in rural America. https://www.nidcd.nih.gov/news/2000/call-hearing-protection-rural-america
ANNE NUGENT GUIGNON, RDH, MPH, CSP, provides popular programs including topics on biofilms, power-driven scaling, ergonomics, hypersensitivity, and remineralization. Recipient of the 2004 Mentor of the Year Award and the 2009 ADHA Irene Newman Award, Anne has practiced clinical dental hygiene in Houston since 1971, and can be contacted at [email protected].
About the Author
Anne Nugent Guignon, MPH, RDH, CSP
ANNE NUGENT GUIGNON, MPH, RDH, CSP, has received numerous accolades over four decades for mentoring, research, and guiding her profession. As an international speaker and prolific author, Guignon focuses is on the oral microbiome, erosion, hypersensitivity, salivary dysfunction, ergonomics, and employee law issues. She may be contacted at [email protected].