My eye's on you: Are dental professionals using safety glasses while rendering care?
BY KANDYCE M. A'SEE, RDH, MS, AND M. SUZANNE MATHIS, RDH, MS
Compared to medicine, dentistry has been slow to consider how patient safety practices can be improved for several reasons. First, the risks of mortality and significant morbidity associated with the practice of medicine are far greater than they are with dentistry.1 In addition, the frequency and severity of adverse events in hospitals have led to campaigns by health authorities, making medical health professionals more aware of certain patient safety needs than dental professionals.
In contrast, dental care is much less structured than hospital care, and most dentists practice in isolation. Many dental professionals are unaware of the safety culture. Nevertheless, incidents can occur in dentistry and can lead to serious consequences.2
According to one study, almost 6% of iatrogenic injuries in dentistry involve patients' eyes.3 Data from the National Reporting and Learning System (NRLS), a voluntary national reporting system set up in 2003 in England and Wales, was analyzed for all incidents of iatrogenic harm in dentistry from January 2009 to December 2009. This data showed that out of 210 incidents of iatrogenic harm to dental patients, 12 injuries involved the eyes.3
Eye protection is part of multiple guidelines on infection control and safety in dental practices. In the "Guidelines for Infection Control in Dental Health-Care Settings 2003," the Centers for Disease Control and Prevention (CDC) requires protective eyewear for both practitioner and patient: "Protective eyewear with solid side shields or a face shield should be worn by dental health-care personnel during procedures and patient care activities likely to generate splashes or sprays of blood or body fluids.
Protective eyewear for patients shields their eyes from spatter or debris generated during dental procedures."4
In addition, the British Dental Association (BDA) published an advice sheet called "Infection Control in Dentistry," which also requires eye protection for both clinician and patient: "Operators and close support clinical staff must protect their eyes against foreign bodies, splatter, and aerosols that may arise during operative dentistry: During scaling (manual and ultrasonic), using rotary instruments, cutting and use of wires, and cleaning instruments. Ideally, protective glasses should have side protection. Patients' eyes must always be protected against possible injury; tinted glasses may also protect against glare from the operating light."5
These guidelines are clear, but not all dental professionals are compliant. In a study published in 2006, Farrier and Gilmour conducted a survey of 200 general dental practitioners at random. The dentists reported their personal use of safety glasses and the use of safety glasses by their patients. Out of the 138 questionnaires returned, 94% of the dentists indicated that they understood the need for protective glasses but only 87% actually wore them.5 Of the 87%, 58% wore their personal glasses, and only 21% of those had proper side protection.5 Only 67% reported compliance with providing safety glasses for adult patients, and 60% reported they would continue to provide dental treatment even if a patient declined to wear any eye protection.5 While dental professionals are aware of the potential risks of not wearing eye protection or not providing eye protection for their patients, and while they are concerned about the possibilities of infections and injuries, the data shows that many still do not wear or provide optimal eye protection.
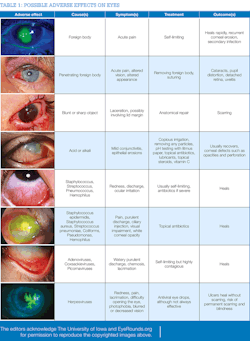
When dental professionals are noncompliant, eye injuries are more likely to occur. The risks includeviral and bacterial contamination of the eye via bodily fluid, as well as trauma (see Table 1).
To further the study of protective eyewear compliance and bring awareness to practicing clinicians about the importance of eye protection, a survey of dental professionals was conducted at the Dental Hygiene Symposium in Savannah, Ga., in July 2015. The purpose of the survey was to determine if clinicians' previous standard precaution training regarding safety glasses affected their adherence to the CDC's guidelines.
GEORGIA SURVEY
All dental professionals, including both dentists and dental hygienists, who participated in continuing education activities at the Annual Dental Hygiene Symposium in Savannah in July 2015 were invited to complete a 12-question survey, enclosed in their course packages, about their usage of safety glasses. The survey also sought to determine if a correlation exists between those who currently wear and provide safety glasses and those who were taught to do so in professional school.
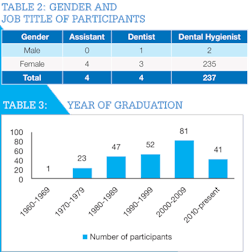
Completion of the survey was considered consent to participate in the study. The questionnaire was approved by the institutional review board (IRB) office and had not been used in previous studies.
Out of the 378 surveys handed out in registration packets, 245 were completed and returned. Of those who returned their surveys, three were male and 242 were female. Four were dentists, four were assistants, and 236 were dental hygienists. One participant had dual titles as a hygienist and assistant (see Table 2). For ease of discussing data, she was categorized as a dental hygienist in Table 2. There was a good crosssection of respondents related to year of graduation (see Table 3).
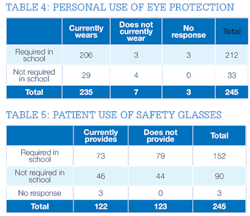
Of the 245 dental professionals who completed the survey, 212 were required to wear safety glasses during dental procedures while attending professional school, and the remaining 33 were not required.
Of the 212 dental professionals who were required to wear safety glasses during professional school, 206 (97%) reported that they currently wear protective eyewear, such as loupes, prescription lenses, or a face shield for various procedures. Three did not respond to indicate whether they currently wear eye protection, and the remaining three indicated that they do not wear any type of eye protection.
Of the 33 who were not required to wear protective eyewear in professional school, four responded that they do not currently wear any type of eye protection, and 29 (88%) indicated that they do (see Table 4). The results of this survey imply that being required to wear eye protection in professional school does not determine if a dental professional will wear it in practice.
Of the 245 participants, 152 reported they were required to provide safety glasses for their patients while attending professional school, but only 73 respondents (48%) are doing so in practice (table 5). Of the 90 respondents who were not required to provide safety glasses to patients while in school, 46 respondents (49%) provide safety glasses for their patients. Of the 245 participants, three did not state if they were required to provide safety glasses while in professional school but indicated that they are currently providing eye protection for their patients. The results of this survey
imply that the school requirement of providing safety glasses for patients does not determine whether dental professionals will provide eye protection in practice.
THE NEED FOR A SAFETY CULTURE
Overall, these results suggest that no correlation exists between the requirement to wear or provide protective eyewear in school and the decision to wear or provide it in practice. Currently, only 50% of the dental professionals surveyed adhere to the CDC's 2003 guidelines by providing their patients with safety glasses (table 4); however, 96% of dental professionals protect their own eyes by wearing safety glasses (table 3).
Promoting a culture of patient safety in dentistry is imperative. The main consideration is the ethical obligation between the health-care provider and the patient. Dental professionals should adhere to the Hippocratic Oath: "First, do no harm." Deciding not to provide protective eyewear can cause harm.
Another consideration is the economic impact on the dental practice. Having effective patient safety measures will reduce the likelihood of an injury and its associated economic costs. A third consideration is the legal security of the dental practitioner. By reducing the likelihood of adverse events by providing safety glasses, the practitioner decreases the probability of legal ramifications.2
The best practices to promote a culture of patient safety are to understand the current situation in regard to patient safety, educate the dental staff regarding the patient safety culture, create safety protocols for staff, establish safety instructions, and share experiences in patient safety with colleagues.2
In addition to adopting new standards of care for the office, patients should be empowered to be their own advocates. Treat patients as though they are part of the dental team by educating them on why eye protection is important and by encouraging them to ask for eye protection if a staff member fails to offer.6
For optimal patient care and limited risks to you, your colleagues, and your patients, embrace the culture of patient safety and follow the CDC's guidelines. RDH
Kandyce M. A'see, RDH, MS, is an assistant professor in the department of dental hygiene at Augusta University, where she serves as co-clinical
coordinator for Patient Care I and teaches Theory and Practice III and Ethics and Practice Management. She also teaches in the online dental hygiene
degree completion program. Kandyce is the author of the children's book, The Tooth Tickler.
M. Suzanne Mathis, RDH, MS, is an instructor in the department of dental hygiene at Augusta University, where she is a clinical instructor and teaches Microbiology. She also teaches in the online dental hygiene degree completion program for the university.
REFERENCES
1. Pemberton MN. Developing patient safety in dentistry. Br Dent J. 2014;217:335-337.
2. Yamalik N, Perez BP. Patient safety and dentistry: What do we need toknow? Fundamentals of patient safety, the safety culture and implementation of patient safety measures in dental practice. Int Dent J. 2012; 62(4):189-196.
3. Thusu S, Panesar S, Bedi R. Patient safety in dentistry - state of play as revealed by a national database of errors. Br Dent J. 2012;213(3):E3,1-8.
4. Centers for Disease Control and Prevention. Guidelines for Infection Control in Dental Health-Care Settings - 2003. MMWR 2003;52(No.RR-17). http://www.cdc.gov/mmwr/PDF/rr/ rr5217.pdf.
5. Farrier SL, Farrier JN, Gilmour AS. Eye safety in operative dentistry - a study in general dental practice. Br Dent J. 2006;200(4):218-223;208.
6. Kelsch N. Jenn's vision: Eye injury prompts dental patient to advocate safety glasses. RDH magazine website. http://www.rdhmag.com/articles/printvolume-34/issue-10/features/jenn-s-vision.html. Published October 16, 2014. Accessed July 15, 2015.
7. http://www.eyerounds.org/