Too many patients are using antibiotics improperly ...and creating a whole new set of problems as a result.
Cynthia R. Biron, RDH
The overuse of antibiotics is increasing bacterial resistance to many of the antibiotics available worldwide. When bacteria are frequently exposed to some antibiotics, they mutate and become resistant to the antibiotics. Antibiotics are over-used and misused in numerous ways.
The Centers for Disease Control (CDC) and the World Health Organization (WHO) have proposed strategies to prevent bacterial resistance to antibiotics. However, adherence to these strategies is another matter ... and questionable.
By far, the most frequent use for outpatient prescription of antibiotics in the United States is otitis media (ear infections). The most common bacterial causes of ear infections are Streptococcus pneumoniae, Haemophilis influenzae, and Moraxela catarrhalis. In 1980, the number and type of prescriptions written for the treatment of ear infections included 4.2 million for amoxicillin and 876,000 for cephalosporin. In 1992, prescriptions for ear infections increased to 12.3 million for amoxicillin, and 6.8 million for cephalosporins.
Most resistant strains of bacteria appear to be a result of overuse of third-generation cephalosporins. The upper-respiratory infections that occur with the common cold or flu are the second most common uses for antibiotics. The manifestations that cause patients to see their physicians for antibiotics include: sore throats, cough, sinus congestion, rhinitis, and bronchitis.
Most respiratory pathogens have become resistant to the commonly prescribed antibiotics, requiring newer, more expensive antibiotics to eliminate these infections. Penicillin- resistant Streptococcus pneumoniae is the greatest problem. In intensive care units of hospitals, there have been increasing reports of antibiotic-resistant pathogens such as methicillin-resistant Staphylococcus aureaus, vancomycin-resistant Enterococcus, and extended-spectrum, beta-lactamase-producing, gram-negative bacilli. Hospitals that have the highest record of reports of resistant strains also have the highest record of antibiotic use. The patients in intensive-care units are five to 10 times more likely to acquire a nosocomial infection than patients in other areas of the hospital.
The overuse and misuse of antibiotics
Ear infections and/or upper respiratory infections related to colds and flu seem to be the prime areas of overuse and misuse of antibiotics. In many instances, antibiotics should not have been prescribed because most colds and flu are caused by viruses, which are not killed by antibiotics. Often, the physician simply surmises that a sore throat is a streptococcus infection and prescribes an antibiotic for it. However, one study showed that, of 517 patients with sore throats who saw their family physician, two-thirds of the antibiotics prescribed were for patients who were culture-negative for streptococcus infection.
A survey of 400 parents indicated that 93 percent believed that antibiotics were necessary for ear infections, 83 percent believed they were needed for throat infections, 32 percent thought they should be prescribed for colds, 58 percent for coughs, and 58 percent thought they were needed for fever. These parents are not happy with their physicians when they do not prescribe an antibiotic to treat ear infections or cold symptoms. In fact, as many as 18 percent of the parents questioned had given their children antibiotics at home before consulting a physician. The antibiotics they had at home were left over from previous prescriptions where the patient had not completed the prescribed regimen.
Parents giving leftover antibiotics from previous prescriptions may be harming their children in two ways:
(1) They may be exposing them to antibiotics that may produce resistant strains of bacteria, rendering such antibiotics useless in the future, and
(2) They may be subjecting their children to the adverse effects of antibiotics that probably were not needed anyway.
The research currently shows that 80 percent of children with ear infections will overcome the symptoms and infection without the use of antibiotics. Yet, 96 percent of pediatricians (n=600) indicated that parents requested antibiotics for their children with ear infections when the antibiotics were not needed. Fifty percent of those pediatricians also said that the parental pressure contributed to antibiotic overuse.
The incorrect selection of types of antibiotics for specific infections leads to an overuse of broad-spectrum antibiotics. If narrow-spectrum antibiotics are used, they may not target the causative agent. So, physicians prescribe a broad-spectrum antibiotic. The appropriate use of narrow-spectrum antibiotics often requires antibiotic sensitivity-testing that is time-consuming and expensive. Now, rapid tests are available for Streptococcus infections of the throat. These tests can be conducted in the physician`s office prior to prescribing an antibiotic.
Are physicians following recommendations?
Two common interventions have been recommended to prevent antibiotic overuse in upper-respiratory infections. They are:
(1) Practice profiling and feedback
(2) Patient education materials
Between July 1, 1996, and Nov. 30, 1997, 216 physicians had their antibiotic-prescribing habits evaluated. In June 1997, they were given the intervention strategies. They were expected to implement them immediately to reduce the amount of antibiotic prescriptions written for upper-respiratory infections. In the July, 1996 to November, 1997 time period, 124,092 episodes of care were noted. Results indicated that the physicians continued to increase the amount of antibiotics prescribed - even after the intervention strategies were implemented! Additional studies have shown that physicians do understand the problem with antibiotic resistance, but their reported practices do not adhere to recently published recommendations.
Are antibiotics overused or misused in dentistry?
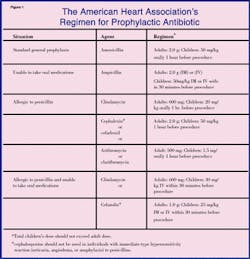
Dental infections often are treated with broad-spectrum antibiotics, such as amoxicillin, but these prescriptions usually are necessary. Dentists prescribe antibiotics when pain, swelling, associated lymphadenopathy, and other signs of infection are present. Dental infections related to tooth decay and periodontitis are bacterial, not viral. If we are following the American Heart Association recommendation to prevent infective endocarditis, we are adhering to the best possible protocol in the interest of our patients and the population in general.
To avoid prescribing prophylactic antibiotics unnecessarily, dentists should refer to the "AHA Recommendations for Cardiac Conditions Associated With Endocarditis" (see Figure 2).
Resistant strains in the oral cavity
If a patient who comes to the dental office is already taking amoxicillin - or any of the antibiotics used for antibiotic prophylaxis against infective endocarditis - the dentist should prescribe a different antibiotic for prophylactic antibiotic rather than increasing the dose of the one the patient is currently taking. Patients who are taking - or have frequently taken amoxicillin - may have oral streptococci that are resistant to amoxicillin, ampicillin, or penicillin. Dentists should prescribe either clindamycin, azithromycin, or clarithromycin for the prevention of endocarditis in such patients. There is a possible cross-resistance with cephalosporins, so this class of antibiotics should also be avoided.
Whenever a patient who requires prophylactic antibiotic against endocarditis has been taking a broad-spectrum antibiotic for some other infection, it is prudent to prescribe a different antibiotic or delay treatment until at least nine-14 days after completion of their current antibiotic regime. This gives the patient`s normal oral flora time to re-establish itself. This also is the reason that patients who require prophylactic antibiotic should have their dental appointments spaced nine-14 days apart.
Take the time to educate your patients about the judicious use of antibiotics. Every health professional must do his or her part to prevent the production of antibiotic-resistant strains of bacteria. Share the information in this article with your patients and others to help with this very real concern for antibiotic effectiveness in our future.
Cynthia R. Biron, RDH, is chair of the dental hygiene program at Tallahassee Community College. She also is a certified emergency medical technician.
References
- Barden LS, Dowell SF, Schwartz B, Lackey C. "Current attitudes regarding use of antimicrobial agents: results from physicians` and parents` focus group discussions."
Clin Pediatr (Phila) 1998 Nov;37(11):665-71
- Braun BL, et al. "Patient beliefs about the characteristics, causes, and care of the common cold: an update." J Fam Prac 2000 Feb;49(20):153-6.
- Conly J. "Controlling antibiotic resistance by quelling the epidemic of overuse and
- isuse of antibiotics." Can Fam Physician 1998 Sep;44:1769-73, 1780-4
- Dagnelie CF, Bartelink ML, van der Graaf Y, Goessens W, de Melker RA
"Towards a better diagnosis of throat infections (with group A beta-haemolytic streptococcus) in general practice." Br J Gen Pract 1998 Feb;48(427):959-62.
- Dajani, AS, et al. "Prevention of bacterial endocarditis recommendations by the American Heart Association." JAMA 1997 June;277:1794-1801.
- F ile TM Jr. "Overview of resistance in the 1990s." Chest 1999 Mar;115(3 Suppl):3S-8S
- Froom, J. et al. "Antimicrobials for acute otitis media? A review from the International Primary Care Network." General Practice 1997 Feb;315:98-102.
- Kotsiou G. "Choosing the right antibiotic." Aust Fam Physician 1998 Oct;27(10):879-82
- Mainous AG 3rd, et al. "An evaluation of statewide strategies to reduce antibiotic overuse." Fam Med 2000 Jan;32(11):22-9.
- Quinn JP. "Clinical strategies for serious infection: a North American perspective."
Diagn Microbiol Infect Dis 1998 Jun;31(2):389-95.
- Spach DH, Black D. "Antibiotic resistance in community-acquired respiratory tract infections: current issues." Ann Allergy Asthma Immunol 1998 Oct;81(4):293-302; quiz 302-3
- Waldrop RD, Prejean C, Singleton R. "Overuse of parenteral antibiotics for wound care in an urban emergency department." Am J Emerg Med 1998 Jul;16(4):343-5
- Weber DJ, Raasch R, Rutala WA. "Nosocomial infections in the ICU: the growing importance of antibiotic-resistant pathogens." Chest 1999 Mar;115(3 Suppl):34S-41S
- Werk LN, Bauchner H. "Practical considerations when treating children with antimicrobials in the outpatient setting." Drugs 1998 Jun;55(6):779-90.
Werk LN, Bauchner H. "Practical considerations when treating children with antimicrobials in the outpatient setting." Drugs 1998 Jun;55(6):779-90.
- Williams DN. "Antimicrobial resistance. Guidelines for the primary care physician."
Minn Med 1998 May;81(5):25-9.
- Zembower TR, Noskin GA, Postelnick MJ, Nguyen C, Peterson LR. "The utility of aminoglycosides in an era of emerging drug resistance." Int J Antimicrob Agents 1998 May;10(2):95-105