Editor's note: This is part one of a two-part series. Read part two.
By now, you have heard something about dental unit waterlines (DUWLs). But you still might be wondering what you’re supposed to do, how the heck you’re supposed to do it, and if it’s even something you have to do.
Spoiler alert: yes, you have to test them. The CDC guidelines say for nonsurgical dental procedures, you should use water that meets the EPA standard for safe drinking water, which is <500 cfu/mL.1 What that means is you need a system in place to ensure the water that goes into your patient’s mouth meets or is below that threshold. The only way to know if your water is safe is to test (more on that soon).
The American Dental Association (ADA) agrees with this,2 and a few states have even passed or are working on legislation to mandate a testing protocol.3,4 Even if your state has not adopted CDC guidelines, as dental professionals, we are required to ensure the care we provide is safe for our patients. Water above 500 cfu/mL is not considered safe. Therefore, offices have been cited by state boards or other entities for violating this standard of care.
Even OSHA is hopping on water safety. While OSHA isn’t focused on patient safety but on employee safety, according to compliance experts familiar with the cases, offices in three different states have been cited under the General Duty clause. This is because the aerosols we create during aerosol-generating procedures (AGPs) come from our DUWLs. A study out of Ohio State University shows that 78% of aerosols come directly from procedural water, and 0% come from patient saliva.5 This is what we are breathing all day long. So, if your water is safe, you’re good to go, but if your water is over 500 cfu/mL, this could adversely affect your health.
Where is your water coming from?
Where to begin? The first thing you need to determine is where the water that comes out of your air/water syringe, handpiece, scaler, etc., is coming from. It might come in from the city plumbing and go directly into your chair. If that’s the case, you have some decisions to make. Your office can install a centralized system to provide an antimicrobial agent into the water to treat the biofilm that grows in the lines. A service tech can install a cartridge into the junction box in the chair that delivers that same antimicrobial agent into the lines. Or you can retrofit the chairs to have a bottle reservoir system. No matter what, there needs to be a way to introduce a product into the dental waterlines to clean and disinfect the lines.
Bottle versus centralized system
There are pros and cons to both bottles and in-line systems. While in-line systems eliminate some of the daily tasks of waterline maintenance, they require a service tech to remediate any issues, and if your area has a boil-water advisory, you must close your doors until the water is safe again.
Dental unit water bottles allow the clinician more autonomy over the water protocol—providing the option to choose from a variety of treatment products, the ability to operate during a boil-water advisory, and shocking the lines as needed. One downside to bottles is running out of water during a procedure.
After weighing the two options, the Association for Dental Safety (ADS) and the ADA recommend dental unit water bottles as the best choice.6,7 However, offices are free to make the decision that is right for them.
Source water
If using a dental unit water bottle, you can choose what water to fill it with. Source water options can include distilled water, store-bought spring water, tap water, or even sterile water (but note that water is no longer considered sterile once it enters your dental unit). It’s important to look at the instructions for use (IFU) for both your chair and treatment product for guidance in determining what water is best for your practice. While many dental professionals think distilled water is the safest, some chair manufacturers are no longer recommending it due to its potentially corrosive effects.
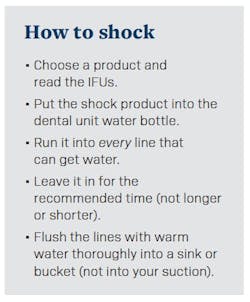
Shock
If all this waterline talk is new to you, shocking is likely where you need to begin. Shocking is using a high-level disinfectant to blast through the biofilm sitting in the DUWLs. There are lots of shock products on the market, and some are stronger than others. Check the IFUs for your dental chair to see if it has product recommendations or products to avoid. Liquid Ultra, ICX Renew, and diluted bleach are the strongest shock products on the market. No matter which product you choose, it is imperative to follow the IFUs or you could damage your chair or not effectively disrupt the biofilm.
Test
Testing is the only way to know (and prove) if your water is below 500 cfu/mL. Once again, check both your chair and treatment product IFUs for a recommended testing regimen. If there is none, ADS recommends testing monthly until you have two consecutive passes and then moving to quarterly testing. If you fail, you start back at monthly.
Much like spore testing, there are mail-in and in-office testing options. Both are effective ways to monitor your DUWLs. Chairside tests are convenient, confidential, and less expensive. Mail-in tests offer third-party validation and more precise results. I personally recommend a mix of the two. Once a year, I perform a mail-in test and utilize in-office tests for the rest.
If selecting a chairside test, it’s essential to follow the steps closely, or you could get an inaccurate result. See Table 1 for hands-on time and how many steps you need to follow. Some tests use a color-change method. If you have difficulty distinguishing color, this might not be the best test for you. Others grow microbes on a paddle. There might be an incubation temperature required. If your room is cold, it might take longer for the microbes to grow.
For mail-in tests, the two most popular methods are R2A and flow cytometry. The R2A method takes the water sample and incubates it on an agar plate. Then, the lab looks for microbial growth in five to seven days. This is considered the gold standard in dental waterline testing. However, flow cytometry is making waves in the testing arena and has proven to be very accurate. This method uses lasers and fluorescence to detect all bacteria, both living and dead. You might think, who cares about dead/damaged bacteria; it’s not going to hurt anyone. Live biofilm loves dead/damaged bacteria to hide in and as a food source. Flow cytometry takes only 20 minutes to get results. So, with the time it takes to mail in your water, you get next-day results.8
No matter what type of test you choose, it’s important to test all the lines that can get water every time you test (whether you use them or not). In fact, a line that can get water but isn’t used regularly is called a dead leg and can often be a source of biofilm. If you will never use that line, have a service tech cap it off at the source, or be sure to flush it regularly.
Once again, when collecting your sample, read the IFUs for the testing method. If it’s a mail-in test, you need to freeze an ice pack for shipping and ensure the lab is open to receive your sample. So, don’t mail it on a Friday or a holiday. Decide if you are testing each line individually or taking a pooled sample. Pooled sampling means taking equal amounts from each line in one operatory.9 If you pass, you know all the lines are good; if you fail, shock all the lines again. Either method is acceptable. The only time I test individual lines is if an op is failing and I’m trying to figure out where the problem is. More on what to do if you fail in my next article.
Stay tuned for part two. While this might sound overwhelming, think of all the things you didn’t know before you entered dentistry. Heck, disinfecting an operatory felt overwhelming in hygiene school, and now we can do that automatically. As we continue the waterline journey in part two, we will discuss interpreting your results, what to do if you fail a test, treating and maintaining DUWLs, and some myths surrounding best practices.
Editor's note: This article appeared in the April/May 2025 print edition of RDH magazine. Dental hygienists in North America are eligible for a complimentary print subscription. Sign up here.
References
- Guidelines for infection control in dental health-care settings – 2003. MMWR; 2003;52(No. RR-17):1–66. https://www.cdc.gov/mmwr/PDF/rr/rr5217.pdf
- Dental unit waterlines. American Dental Association. https://www.ada.org/resources/ada-library/oral-health-topics/dental-unit-waterlines
- Washington Administrative Code (WAC). 246-817-660. February 5, 2025. Washington State Legislature. https://app.leg.wa.gov/wac/default.aspx
- Board of Dentistry issues notice of intent to adopt dental unit water quality rule. Georgia Dental Association. December 20, 2024. https://www.gadental.org/news-details/2024/12/20/board-of-dentistry-issues-notice-of-intent-to-adopt-dental-unit-water-quality-rule
- Meethil AP, Saraswat S, Chaudhary PP, Dabdoub SM, Kumar PS. Sources of SARS-CoV-2 and other microorganisms in dental aerosols. J Dent Res. 2021;100(8):817-823. doi:10.1177/00220345211015948
- Dental unit waterline fact sheet. Association for Dental Safety. https://www.myads.org/topics-duwl-dental-unit-waterline-fact-sheet
- Dental unit water lines. American Dental Association. https://www.ada.org/resources/practice/legal-and-regulatory/ 04_dental-unit-water-lines
- Carey CM, Mills SE, Vigil R, Aungst M, Favazzo L. Application of flow cytometry to analyze microbial quality of dental unit water. JADA Found Sci. 2024;3:100037. doi:1016/j.jfscie.2024.100037
- Mills S, Porteous N, Zawada J. Dental unit water quality: Organization for Safety, Asepsis and Prevention white paper and recommendations—2018. J Dent Infect Control Safety. 2018;1(1):1-12.