As dental hygienists, we are deeply invested in our patients’ overall well-being and oral health. We understand that good nutrition is fundamental, and a nuanced understanding of how vitamins and minerals impact oral health elevates our expertise and patient care.
It’s undeniable that the food we consume directly affects our oral health. Micronutrients, including vitamins and minerals, are the essential building blocks of healthy oral tissues.1,2 Any imbalance in these micronutrients can lead to a variety of oral health problems.
With the rise of the “self-care” movement, many people are turning to supplements without seeking professional guidance. This trend presents unique challenges for us as health-care providers:
- Ambiguity in self-medication: The very definition of “self-medication” remains unclear, making it difficult to gather reliable data and understand its full scope.
- Lack of disclosure: Patients may not always be forthcoming about their supplement use, potentially withholding crucial information about their health.
- Absence of a tracking system: A standardized system for monitoring micronutrient use would make it easier to assess its impact on individual and overall oral health.
By proactively and comprehensively addressing micronutrient self-
medication, we can deliver the highest-quality care to our patients and contribute significantly to their overall well-being.
The power of micronutrients
Vitamin A (retinol) is essential for maintaining the integrity of the oral mucosa. It promotes the differentiation and proliferation of epithelial cells, which form a protective barrier against microbial invasion and inflammation.3,4 Additionally, it supports healthy salivary gland function, ensuring adequate saliva production for lubrication, digestion, and the clearance of debris and bacteria, thus reducing caries risk.
- Deficiency can lead to xerostomia, dental defects, and exacerbated periodontal disease.
- Hypervitaminosis A can cause oral ulcerations and jawbone issues.
- Sources: Leafy green vegetables, carrots, fish liver oil, and dairy products
Vitamin C (ascorbic acid) plays a critical role in periodontal health due to its involvement in collagen synthesis. Collagen is an essential structural protein in connective tissues, providing strength and integrity to the gingiva and periodontal ligament.5 Adequate levels are, therefore, vital for maintaining healthy gingival tissues and their ability to withstand mechanical and inflammatory insults.6,7
- Deficiency can lead to gingival bleeding, inflammation, and periodontitis.
- While excess intake is generally not a concern, extremely high doses may indirectly contribute to enamel erosion due to increased gastric acid production.
- Sources: Citrus fruits (oranges, grapefruits, lemons), berries (strawberries, blueberries, raspberries), and tomatoes
Vitamin D plays a crucial role in oral health by facilitating calcium absorption, essential for strong teeth and bones. It also exhibits anti-inflammatory properties that benefit periodontal tissues. A study by Kim et al. highlighted a significant association between low serum vitamin D and tooth loss and severe periodontitis in Koreans aged 50 and older, underscoring the importance of monitoring vitamin D levels for oral health.8,9
- Deficiency can lead to weakened enamel, delayed tooth eruption, and an increased risk of periodontitis. For example, children with dental rickets may experience nonsyndromic amelogenesis and dentinogenesis imperfecta.
- Excessive vitamin D intake can disrupt enamel formation and cause calcification of the salivary glands.
- Sources: Sunlight is the main source of vitamin D, but it can also be obtained through diets rich in fatty fish, fortified foods, and certain meats.
Vitamin E (α-tocopherol) is a potent antioxidant whose primary function is to protect the gingival tissues from oxidative stress and inflammation, but beyond its protective role, vitamin E also contributes to several important processes in the oral cavity; for example, it aids in bone formation by mitigating the damaging effects of free radicals on cells. This, in turn, positively influences tooth development and overall oral health. Furthermore, vitamin E supports efficient wound healing in the oral cavity, facilitating tissue repair and regeneration following injury or surgical procedures.10,11
Emerging research suggests that vitamin E may also play a role in preventing oral cancer. Its antioxidant properties help neutralize free radicals, which damage cells and potentially lead to cancerous changes. A study by Iqubal et al.12 highlighted the significant role of vitamin E in preventing oral cancer due to its ability to neutralize free radicals and inhibit the formation of nitrosamines, carcinogens often found in tobacco products.
- Deficiency can exacerbate inflammatory conditions such as oral lichen planus (OLP) and can compromise overall oral health.
- Although rare, its excessive intake, primarily through high-dose supplementation, can impair blood clotting.
- Sources: Nuts, seeds, and vegetable oils
B vitamins (B6–pyridoxine and B12–cobalamin) play a vital role in preserving the integrity of the oral mucosa and supporting the proper function of the nerves that innervate the oral cavity. They also facilitate the healing of mucosal tissues and support the maintenance of healthy bone, both critical for recovery from periodontitis.13
- When B vitamin levels are insufficient, patients may present with a range of oral conditions, including glossitis, angular cheilitis, and burning mouth syndrome. Furthermore, studies have explored the connection between vitamin B12 deficiency and specific oral conditions such as OLP. A study by Chen et al.14 found that patients with OLP had a significantly higher likelihood of vitamin B12 deficiency compared to healthy individuals. This suggests that adequate B12 levels may be significant for managing OLP. Another study by Sun et al.15 investigated the link between vitamin B12 deficiency and canker sores. Their findings indicated a significant association between low B12 levels and the occurrence of these painful ulcers.
- Sources: Meat, poultry, fish, eggs, dairy products, and leafy green vegetables
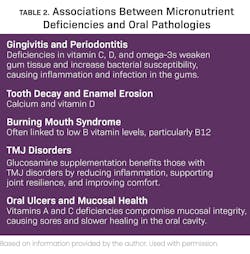
Micronutrients can also have an impact on drug interactions (table 1) as well as associations between micronutrient deficiencies and oral pathologies (table 2).
Supplements: Adjunctive support for oral health
Beyond essential vitamins, certain supplements can provide added benefits for oral health.
Omega-3 fatty acids are essential polyunsaturated fats that offer a multitude of health benefits, including significant support for periodontal health. Their potent anti-inflammatory properties play a crucial role in managing periodontal disease by effectively reducing gingival inflammation and mitigating alveolar bone loss. A study published by Kesavalu et al.16 provided compelling evidence for the benefits of omega-3 in periodontal health. The researchers demonstrated that a diet enriched with fish oil significantly reduced alveolar bone loss in rats compared to a control group. This finding suggests that omega-3s can help maintain the integrity of the bone supporting the teeth, thus contributing to the prevention of tooth loss.17
The therapeutic effects of omega-3 fatty acids in periodontal disease are attributed to their ability to:
- Modulate inflammatory pathways: Omega-3s can inhibit the production of pro-inflammatory molecules, thereby reducing the inflammatory response in periodontal tissues.
- Promote tissue resolution: Omega-3s can stimulate the production of specialized pro-resolving mediators (SPMs), which actively promote the resolution of inflammation and tissue repair.
- Improve blood flow: Omega-3s can enhance circulation in periodontal tissues, facilitating nutrient delivery and waste removal.
Glucosamine, an amino sugar that is a fundamental building block of cartilage and synovial fluid, has garnered attention for its potential benefits in managing temporomandibular joint (TMJ) disorders.18 Its therapeutic effects are attributed to two primary mechanisms:
- Cartilage support: Glucosamine stimulates the metabolic processes involved in cartilage formation and maintenance, promoting the health and integrity of the joint structures.
- Anti-inflammatory action: Glucosamine exhibits anti-
inflammatory properties that help counteract the breakdown of cartilage caused by inflammation, a common factor in TMJ disorders.
This combined effect translates to reduced pain and improved mobility for patients, offering a potential avenue for alleviating the discomfort and functional limitations often associated with degenerative joint conditions such as TMJ osteoarthritis.19
Integrating nutritional counseling into patient care
While we are not registered dieticians, we can play a significant role in educating patients about the connection between nutrition and oral health. Here are some practical tips:
- Dietary assessment: Incorporate simple questions about diet and supplement use during patient intake.
- Targeted recommendations: Provide specific recommendations for foods rich in the vitamins and minerals crucial for oral health.
- Supplement guidance: Offer guidance on appropriate supplement choices and dosages, emphasizing the importance of consulting with a health-care provider or registered dietician.
- Collaboration: Maintain open communication with patients’ physicians and other health-care providers to ensure a comprehensive and coordinated approach to overall health.
The integration of micronutrient knowledge into dental hygiene practice represents an exciting opportunity to elevate our profession. By becoming experts in the nutritional aspects of oral health, we can provide a higher level of care and solidify our role as essential partners in overall wellness.
Editor's note: This article appeared in the January/February 2025 print edition of RDH magazine. Dental hygienists in North America are eligible for a complimentary print subscription. Sign up here.
References
- Shetty AS, Shenoy R, Bajaj PD, et al. Role of nutritional supplements on oral health in adults – a systematic review. F1000Res. 2023;12:492. doi:10.12688/f1000research.134299.1
- Lešić S, Ivanišević Z, Špiljak B, Tomas M, Šoštarić M, Včev A. The impact of vitamin deficiencies on oral manifestations in children. Dent J (Basel). 2024;12(4):109. doi:10.3390/dj12040109
- Gossweiler AG, Martinez-Mier EA. Chapter 6: Vitamins and oral health. Monogr Oral Sci. 2020;28:59-67. doi:10.1159/000455372
- Fageeh HN, Fageeh HI, Prabhu A, Bhandi S, Khan S, Patil S. Efficacy of vitamin C supplementation as an adjunct in the non-surgical management of periodontitis: a systematic review. Syst Rev. 2021;10(1):5. doi:10.1186/s13643-020-01554-9
- Wang J, Fan Y, Qian J, et al. Relationship between dietary fiber and vitamin C intake and oral cancer. Front Public Health. 2022;10:880506. doi:10.3389/fpubh.2022.880506
- Li W, Song J, Chen Z. The association between dietary vitamin C intake and periodontitis: result from the NHANES (2009-2014). BMC Oral Health. 2022;22(1):390. doi:10.1186/s12903-022-02416-7
- Ustianowski Ł, Ustianowska K, Gurazda K, Rusiński M, Ostrowski P, Pawlik A. The role of vitamin C and vitamin D in the pathogenesis and therapy of periodontitis–narrative review. Int J Mol Sci. 2023;24(7):6774. doi:10.3390/ijms24076774
- Stein SH, Livada R, Tipton DA. Re-evaluating the role of vitamin D in the periodontium. J Periodontal Res. 2014;49(5):545-553. doi:10.1111/jre.12149
- Kim H, Shin MH, Yoon SJ, et al. Low serum 25-hydroxyvitamin D levels, tooth loss, and the prevalence of severe periodontitis in Koreans aged 50 years and older. J Periodontal Implant Sci. 2020;50(6):368-378. doi:10.5051/jpis.2002540127
- Xin J, Jiang X, Ben S, et al. Association between circulating vitamin E and ten common cancers: evidence from large-scale Mendelian randomization analysis and a longitudinal cohort study. BMC Med. 2022;20(1):168. doi:10.1186/s12916-022-02366-5
- Reppuccia S, Crocetto F, Gragnano E, et al. Oil-based vitamin E oral spray for oral health in pregnancy. Future Sci OA. 2022;8(4):FSO790. doi:10.2144/fsoa-2021-0095
- Iqubal MA, Khan M, Kumar P, Kumar A, Ajai K. Role of vitamin E in prevention of oral cancer:–a review. J Clin Diagn Res. 2014;8(10):ZE05-ZE07. doi:10.7860/JCDR/2014/9166.4958
- Nolan A, McIntosh WB, Allam BF, Lamey PJ. Recurrent aphthous ulceration: vitamin B1, B2 and B6 status and response to replacement therapy. J Oral Pathol Med. 1991;20(8):389-391. doi:10.1111/j.1600-0714.1991.tb00950.x
- Chen HM, Wang YP, Chang JYF, Wu YC, Cheng SJ, Sun A. Significant association of deficiencies of hemoglobin, iron, folic acid, and vitamin B12 and high homocysteine level with oral lichen planus. J Formos Med Assoc. 2015;114(2):124-129. doi:10.1016/j.jfma.2014.10.004
- Sun A, Chen HM, Cheng SJ, et al. Significant association of deficiencies of hemoglobin, iron, vitamin B12, and folic acid and high homocysteine level with recurrent aphthous stomatitis. J Oral Pathol Med. 2015;44(4):300-305. doi:10.1111/jop.12241
- Kesavalu L, Vasudevan B, Raghu B, et al. Omega-3 fatty acid effect on alveolar bone loss in rats. J Dent Res. 2006;85(7):648-652. doi:10.1177/154405910608500713
- Papathanasiou E, Alreshaid R, de Godoi MA. Anti-inflammatory benefits of food ingredients in periodontal diseases. Pathogens. 2023;12(4):520. doi:10.3390/pathogens12040520
- Derwich M, Górski B, Amm E, Pawłowska E. Oral glucosamine in the treatment of temporomandibular joint osteoarthritis: a systematic review. Int J Mol Sci. 2023;24(5):4925. doi:10.3390/ijms24054925
- Jerosch J. Effects of glucosamine and chondroitin sulfate on cartilage metabolism in OA: outlook on other nutrient partners especially omega-3 fatty acids. Int J Rheumatol. 2011;2011:969012. doi:10.1155/2011/969012