Bridging the gap: How periodontal health influences hypertension and overall wellness
Dental care offers more insights into our patients' heart health than we previously understood. More than a decade of evidence-based research proves the profound connection between periodontal health and cardiovascular conditions, particularly hypertension. This involves intricate biological pathways where inflammation is a critical intermediary, directly linking periodontal health to heart health.
Delving into this relationship not only reshapes the understanding of dental care but also highlights the importance of integrated health strategies in preventing and managing systemic diseases. Maintaining healthy gums could be vital to controlling blood pressure and enhancing heart health.
The American Heart Association states a normal blood pressure reading is less than 120/80 mm Hg. A reading of 120-129/less than 80 mm Hg is considered elevated blood pressure, while a reading of 130-139/80-89 mm Hg is classified as stage 1 high blood pressure. Stage 2 high blood pressure is a reading of 140/90 mm Hg or higher. Patients must understand these numbers and work with their health-care providers to manage their blood pressure.1
Periodontal disease is not merely a local oral health issue but a significant contributor to systemic health problems, including hypertension.2 Characterized by chronic inflammation, periodontal disease extends its impact beyond the oral cavity, influencing systemic circulation and contributing to endothelial dysfunction, a critical factor in the development of hypertension. This dysfunction is mediated by inflammatory cytokines such as TNF-alpha and IL-6, alongside an increase in C-reactive protein, all known to advance the progression of atherosclerosis.
The bacteria responsible for periodontal disease can enter the bloodstream, inducing direct vascular damage and promoting the formation of atherosclerotic plaques. Thus, maintaining optimal oral hygiene and regular dental checkups is crucial for reducing the burden of these bacteria and their associated inflammatory mediators.
Salivary diagnostics
Advancements such as salivary diagnostics are revolutionizing the early detection and management of periodontal disease and hypertension. This innovative approach involves analyzing saliva to detect pathogenic bacterial loads and biomarkers associated with systemic diseases, offering a noninvasive method to rapidly assess someone’s health status.
Research has shown that patients with high levels of oral bacteria on their DNA test tend to have high blood pressure, even if they don't show signs of active periodontal disease.3 Therefore, checking a patient's blood pressure during every dental appointment is crucial. By integrating salivary diagnostics into routine dental visits, health-care providers can identify risk factors for hypertension early and implement timely interventions.
Screening and managing patients with hypertension require special attention. The primary concern during treatment is the possibility of a sudden, acute increase in blood pressure, which could lead to serious complications such as stroke or seizure. This increase in blood pressure can be triggered by emotional stress or pain, which stimulates the sympathetic nervous system. Take precautions to ensure a safe and successful treatment.
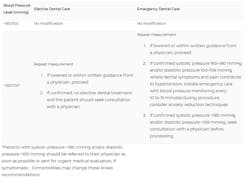
Retake your patient's blood pressure readings after a five-minute interval if it’s elevated. If the readings remain high, suggest reappointing the scheduled appointment. Remember to share the readings with the patient and encourage them to follow up with their health-care providers. Figure 1 shows ADA guidelines for hypertension patients and when it’s safe to continue with dental care.4
Answer these two questions before commencing dental hygiene treatment: what are the patient's risks if they proceed with treatment? What blood pressure level is unsafe for proceeding with the scheduled treatment?
Antihypertension medications
Review your patient's health and pharmacological history. There are many oral side effects of antihypertensive medications. These may include5:
- Chronic cough (e.g., angiotensin converting enzyme inhibitors [ACEIs], as well as direct renin inhibitors)
- Taste changes (e.g., ACEIs, beta blockers, alpha-adrenergic blockers, and calcium channel blockers [CCBs])
- Loss of taste (e.g., ACEIs and angiotensin II receptor blockers [ARBs])
- Angioedema of lips, face, and tongue (ACEIs and ARBs)
- Upper respiratory tract infections (e.g., ARBs)
- Gingival hyperplasia/overgrowth (e.g., CCBs)
- Dry mouth (e.g., thiazide diuretics and alpha-adrenergic blockers)
- Lichenoid reactions6 (e.g., thiazide diuretics and beta blockers)
- Lupuslike oral and skin lesions (e.g., direct vasodilators)
- Parotid pain (e.g., central alpha-adrenergic [alpha 2] agonists)
Observe the overall picture
When evaluating a patient's risk for hypertension, consider their diet, lifestyle, quality of sleep, and oral hygiene/periodontal status. Dental hygienists can play a vital role in promoting overall health by screening for obstructive sleep apnea (OSA) and hypertension. Early identification can lead to timely interventions and referrals, potentially improving patients’ overall health outcomes.
Diet and physical activity are pivotal in managing periodontal disease and hypertension. Anti-inflammatory diets, such as the Mediterranean diet, reduce systemic inflammation and improve oral and vascular health. Regular physical activity enhances cardiovascular fitness and endothelial function, decreases inflammatory markers, and improves overall health, helping to alleviate symptoms of periodontal disease and reduce blood pressure.6
The selection of appropriate oral home care products is critical. The oral microbiome influences nitric oxide, a vasodilator involved in blood flow regulation. Certain oral care products can disrupt this microbiome and negatively impact nitric oxide production.7 Choosing products that support the health of the oral microbiome and enhance nitric oxide production can be particularly beneficial for patients with hypertension.8
The relationship between periodontal disease and hypertension is complex, emphasizing the importance of a comprehensive approach to health care that involves both dental and medical professionals. Dental practitioners can identify patients at risk for hypertension before symptoms become apparent, potentially preventing long-term damage. Effective management of periodontal disease can lead to better blood pressure control and a reduced risk of cardiovascular diseases, stressing the importance of holistic patient care that considers the broader impact of oral health on systemic conditions.
Editor's note: This article appeared in the July 2024 print edition of RDH magazine. Dental hygienists in North America are eligible for a complimentary print subscription. Sign up here.
References
1. Understanding blood pressure readings. American Heart Association https://www.heart.org/en/health-topics/high-blood-pressure/understanding-blood-pressure-readings
2. Macedo Paizan ML, Vilela-Martin JF. Is there an association between periodontitis and hypertension? Curr Cardiol Rev. 2014;10(4):355-361. doi:10.2174/1573403x10666140416094901
3. Desvarieux M, Demmer RT, Jacobs DR Jr, et al. Periodontal bacteria and hypertension: the oral infections and vascular disease epidemiology study (INVEST). J Hypertens. 2010;28(7):1413-1421. doi:10.1097/HJH.0b013e328338cd36
4. Hypertension. High blood pressure. American Dental Association. https://www.ada.org/en/resources/ada-library/oral-health-topics/hypertension
5. Fact sheet: hypertension in children & adolescents. College of Dental Hygienists of Ontario. April 18, 2023. https://cdho.org/factsheets/hypertension-in-children-adolescents/
6. Radić J, Vučković M, Gelemanović A. et al. Interconnectedness between periodontitis stage, oral hygiene habits, adherence to the Mediterranean diet and nutritional status in Dalmatian kidney transplant recipients: a cross-sectional study. Sci Rep. 2022;12(1):11614. doi:10.1038/s41598-022-15589-6
7. Bryan NS, Tribble G, Angelov N. Oral microbiome and nitric oxide: the missing link in the management of blood pressure. Curr Hypertens Rep. 2017;19(4):33. doi:10.1007/s11906-017-0725-2
8. Blot S. Antiseptic mouthwash, the nitrate-nitrite-nitric oxide pathway, and hospital mortality: a hypothesis generating review. Intensive Care Med. 2021;47(1):28-38. doi:10.1007/s00134-020-06276-z
About the Author

Kerry Lepicek, RDH
With more than 20 years of clinical experience, Kerry Lepicek, RDH, is an international lecturer on oral biofilm, halitosis, oral-systemic connection, and the dental hygiene process of care. She is the editor for The Hygiene Corner with Women in Dentistry, serves on the advisory board for the American Academy for Oral Systemic Health, and is a cast member on The RDH View. Kerry recently received the Award of Distinction from the Ontario Dental Hygienists Association. Reach her at [email protected].

Machell Hudson-Hoover, RDH, CHC, FAAOSH
Machell Hudson-Hoover, RDH, CHC, FAAOSH, is the founder and CEO of Integrative Dental Coaching, as well as the head of Oral Systemic Health and Hygiene Growth for the Clinical Calibration Institute. Her mission is to support dental and medical health care professionals in transforming care from a reactive "sick care" approach to a proactive, health-minded approach. Machell is fiercely passionate about dental hygiene and is devoted to showcasing the crucial role dental professionals play as frontline leaders in healthcare, advocating for the profound impact of oral health on overall well-being. Machell can be reached at [email protected].