by Sandy Sheffler
I entered dental hygiene 30 years ago because I like people and have a caring nature. It seemed to be the perfect fit. In the dental hygiene curriculum, we learned a lot of scientific information such as microbiology. But 30 years ago, the emphasis in dental hygiene programs and dental practices throughout the United States was primarily on cleaning teeth.
At the time, the "science" of dental hygiene was limited to scaling and polishing, and little importance was placed on the scientific rationale of why we were performing these clinical skills.
This may seem a bit unusual, but I have worked in the same dental practice for 25 years. About 15 years ago, my dentist/employer, Dr. Barry Buchman, searched for better answers for our patients who were not maintaining well, even after periodontal surgery. His search led us to Dr. Paul Keyes and Bill Landers, president of OraTec Corp., who showed us that periodontal disease was actually a bacterial infection.
Dr. Buchman purchased a phase contrast microscope with a monitor, and we began our quest to treat our patients more effectively. At the time, we had no idea where this new approach to dental care and patient education would take us.
Using a phase contrast microscope to view oral bacteria was a novel idea to most patients and dental professionals 15 years ago. Fortunately, I was in a fee-for-service practice, seeing adult patients every 45 minutes. After implementing the microscope, I saw each patient for an hour. It became apparent that I would need more time with patients to educate them on why and how we were treating their gingival and periodontal diseases. It was at this time that my career took a more positive direction and I realized there was no turning back.
How using phase contrast microscope works
First, we began taking microscopic plaque samples from all of our patients. We allowed each patient to view his or her slide on the microscope. It was very interesting to see patients' reactions when they saw the moving organisms from their oral cavity. They asked, "What can we do about this?" "Is this really from my mouth?" Without any prompting from us, they were concerned and took responsibility for their mouths.
Based on our initial experiences, we set up a system to compare the pocket depths, radiographic findings, and microscopic risk factors, and presented a plan to treat their periodontal infection. By increasing our periodontal treatment with root planing and subgingival irrigation, the microscope paid for itself within three months.
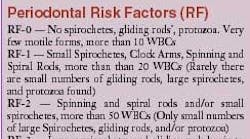
I explain to patients that we work as a team. I place no blame for the periodontal infection on my patients. I let them know that I can only do so much with an anti-infective professional regimen, and that the rest is up to them. Together, we can achieve a healthy mouth during several appointments. Our protocol depends on the severity of their periodontal condition. I determine how many appointments they will need based on the Perio Case Type (PCT) and the microscopic Risk Factor (RF). The RF is determined on a scale of 0-4.
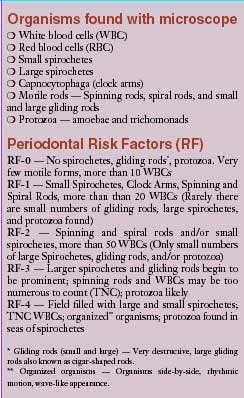
On a microscopic sample, the key organisms are white blood cells, spirochetes, and various types of motile rods. We also view amoeba and occasionally trichomonads. If a patient has a Perio Case Type 1 and Risk Factor 0, then they are not considered a periodontal patient. I perform a traditional prophylaxis, fine tune their home care, and set a six-month re-care appointment. For these patients, I will do a microscopic exam every five years when their full mouth series (FMS) of radiographs is updated, unless there is periodontal change before that.
The more serious conditions, a PCT 3-4 or RF 3-4, require seven to nine appointments. The dentist and hygienist evaluate the conditions at the new patient exam. The patients then return for a consultation/treatment plan appointment, where we tell them they will require periodontal treatment. The first periodontal appointment takes 90 minutes. I perform a full-mouth debridement using an ultrasonic scaler that has an antibacterial agent flowing through it. Following the debridement, I work with my patients on home care.
The remaining appointments include microscopic sampling, ultrasonic scaling with antiseptic, traditional scaling and root planing (SRP), and subgingival irrigation (using a professional model of Viajet) with an antibacterial agent. Each appointment takes one hour. The patients with severe cases take an hour per quadrant, while the less severe take an hour for two quadrants.
After SRP is completed, my patients return two or three times for microscopic exams and full mouth irrigation. Throughout the process, the microscopic monitoring is very important. We can see if there has been a reduction of bacteria and assess if the treatment and homecare is succeeding. The final appointments determine if the patient is ready to go on maintenance. We want the slides to be risk-free by the end of the SRP appointments to be sure the patient can maintain the results. These patients are then seen in three to four month intervals for periodontal maintenance.
The use of the microscope keeps my patients involved. They want to view their progress, and the memory of the "bugs swimming in my mouth" motivates them to continue their daily oral care.
The microscope can also be used preventively with young people, as well as with older patients who show high risk microscopically with no bone loss and normal probing depths. Preventively, it is much better to start off with a regimen to eliminate the harmful bacteria. This involves either oral irrigation or a rubber-tip stimulator with a paste mixture of baking soda and water. After viewing the organisms on the microscope, young people want to prevent dental diseases rather than risk clinical and radiographic signs of destruction.
Home care
Home oral irrigation is a priority for my patients. Like most hygienists, I learned many variations in home-care techniques and about a variety of interproximal aids. I spent years promoting dental floss and met resistance from many patients. When I began using the microscope, I realized that even patients who used dental floss were not thoroughly removing high-risk bacteria from the base of the pockets. Many of my patients who rinsed daily with an antiseptic mouthwash still showed a high bacterial risk on the microscopic slide.
The author and microscope in her operatory.
We dispense the Viajet irrigator in our office. The unit provides two types of tips - a standard tip that jets the liquid towards the gingiva that is highly effective for PCT 1-2, and a Sulcasoft(tm) tip that is inserted subgingivally to allow the irrigant to flow to the base of the pocket. We used to think that the force of the jet would cause damage to the gingiva, but it has been my experience with hundreds of patients that this is not true. My patients have become very compliant and skilled. There are some who actually attach a cannula tip onto an adapter and insert the tip subgingivally to irrigate 7+mm pockets. I dispense chlorhexidine (CHX), and then switch to TheraSol, herbals (Under the Gum), and even baking soda.
Suggested irrigants
I use a number of different oral irrigants with my patients, then monitor their success with the microscope. For in-office irrigation, we make a diluted 0.2 percent chlorhexidine solution, which we order from an independent pharmacy that carries a license to dispense CHX in a 5 percent solution. We also use an herbal product called Under the Gum in the ultrasonic scaler, as well as TheraSol.
The professional model Viajet is furnished with a heater, which I use after scaling. I use a two-step process with the irrigants. With the ultrasonic, used for debridement, I prefer to use a solution with a more pleasant taste. CHX is extremely effective, but even when flavored tends to unfortunately taste unpleasant. Therefore, I follow my scaling with CHX in the Viajet and suction as I irrigate to prevent the patient from swallowing or tasting too much solution. For some of my patients I irrigate in-office with an endo syringe using povidone iodine and distilled water at a 50/50 dilution (assuming they don't have an iodine allergy). I use iodine when the bacteria seem to be resistant and I want to bring the bacterial count down quickly.
Other influencing factors
Many factors inhibit the reduction of bacteria. The immune system plays an important part in healing. A patient whose health is compromised in some way will not respond to therapy as quickly as a healthy individual. Smoking and stress also inhibit progress.
The periodontal condition of a mate or spouse can affect results. Since re-infection can occur, it is helpful if both partners are monitored. All care is done on an individual basis. There is some trial-and-error that is monitored microscopically. The microscope is a useful guide to modify the home-care plan for maximum results. If a particular home-care plan is not controlling the microflora, I can change it immediately rather than wait three to six months to see if there has been any additional loss of attachment.
Products to consider are:
• Irrigators - Viajet Personal Irrigator (purchased through OraTec); Viajet Professional Irrigator for in-office use (OraTec); Waterpik (purchased in retail stores)
• Irrigants - Chlorhexidine 5 percent solution (pharmacies with license to dispense); TheraSol (OraTec); Under the Gum (Dental Herb Company); baking soda; and povidone iodine (pharmacy)
• Cannula tips and adapters for Viajet (OraTec)
Case presentations
One advantage to working in the same office for many years is the ability to track patients' progress. I have chosen to highlight below three patients whom I've worked with very closely for many years. Two of the three have been patients of the practice for more than 30 years. We began anti-infective therapy and microscopic monitoring in 1989, and periodontal damage had already occurred.
• Patient #1 - The first patient is a 54-year-old, white, non-smoking female who has been a patient since 1974, when she had four teeth with 5 mm pockets. Her home care at the time consisted of brushing and flossing. By 1988, three teeth had 8+mm pockets and six teeth had 5mm pockets. In 1988, she lost teeth numbers 19 and 30, which were replaced by fixed bridges.
In 1990, the first microscopic exam was performed with a RF-3. We performed four quadrants scale and root plane with debridement and irrigation. Homecare included Waterpik with water and Pocket Care Irrigator (24 gauge) with CHX to be used in the deep pockets.
By 1995, the patient still had two sites with pocket depths of 7mm and 5mm. A complete occlusal equilibration was done in 2000. As of 2003, there was only one site of 5mm and no additional tooth loss.
This patient is extremely compliant, adheres to daily irrigation, and is seen every three months. She has microscopic exams each time at her request. For the most part, all of her slides have been negative. Occasionally, the deepest areas will show some increase in bacteria. In these sites, I'll use an adjunct such as Arestin and modify the irrigant that she uses.
• Patient #2 - The second patient I tracked is a 46-year-old, white male who smokes. He has been a patient since 1966. In 1972, the first indication of periodontal changes was detected clinically. Home-care instructions for plaque control consisted of disclosing tablets, brushing, and flossing. This patient had a tough time through his teenage years and he was not compliant. Many teeth were decayed.
I first saw him in 1979, and the tissue bled upon touch. Between 1982 and 1988, his periodontal condition deteriorated. By 1988, there were four sites with 10mm pockets, three sites with 8mm pockets, and 15 sites with 5 to 6 mm pockets. This patient most likely had juvenile periodontitis; however, it was not defined as such in his records.
Scaling and curettage, as well as a complete occlusal equilibration, were performed by the dentist in 1989. Clenching had also been a factor.
In 1990, the first microscopic exam was taken (rated as RF-3), and full-mouth root planning and irrigation with an antimicrobial was performed. The patient was prescribed metronidizole. By 1991, he began using a product called OraChlor in his irrigator three times per week, and peroxide on a ProxyBrush in the deeper areas. We moved on to Hibiclens (CHX) in 1993, and by then he was irrigating five times a week. The microscopic slide was negative.
In 1993, a new FMS and complete charting showed four sites of 5mm pockets and three sites with 7mm pockets. Tooth #14, which had one of the 10mm sites, was eventually extracted and replaced with a three-unit bridge. FMS were taken every three years. In 2002, Arestin was used for #3 distal/lingual, and in 2003 number 19 was extracted after a failed root canal and replaced with a bridge.
This patient's parents are both edentulous. Gingival recession has progressed since 1998. This patient was never interested in wearing a night guard; however, his slides have been mostly negative for years. All pockets are within normal limits except for #3 distal with a 6mm pocket, #3 lingual with a 7mm pocket, and #2 with a 5mm pocket.
Fortunately, he stopped smoking in January 2004. This patient is very compliant, is seen every three months, and prognosis is very positive for his remaining teeth.
• Patient #3 - This last patient has a different story. He is a 54-year-old, non-smoking white male. He became a patient in 1991. He had prior periodontal disease and was searching for an alternative to the periodontal surgery that had been recommended. He had pocket depths in five sites 8 to 10mm, and six sites with 5mm (microscopic RF-4).
Treatment consisted of full-mouth debridement, four quadrants SRP, and oral irrigation. A complete occlusal equilibration was also performed. His home-care instructions included oral irrigation using a Viajet with Hibiclens 1:30 dilution.
After therapy, the periodontal pockets were reduced, leaving three sites with 8 to 10mm and two sites with 5mm pockets. From 1995 to 1997, there were several 5mm depths and three 7 mm pockets (microscopic RF-0).
The latest FMS was taken in 2002. (FMS is taken every three to four years). No teeth have been lost. There are still two sites at 7mm, two sites at 6mm, and one 5mm site that have remained microscopically negative since the initial treatment. One site, buccal furcation number 14, has been symptomatic, however the tooth is not mobile and re-treatment has stabilized the infection.
This patient is highly motivated. He was not interested in periodontal surgery nor did he want to lose any teeth. He irrigates his mouth daily with water and uses Hibiclens three times a week. In the remaining deep areas he uses a 24-gauge cannula tip. He is seen on a three-month schedule.
Continuing education
I have taken many courses from experts in the area of anti-infective therapy. The learning curve with anti-infective therapy is continuous, and I have revised my treatment modalities over the years.
When I first started using the microscope and irrigation solutions, there were not many irrigating options. Now, I primarily use Under the Gum in my ultrasonic scaler and sub gingival irrigation with either CHX or TheraSol. I also use diluted povidone iodine with an endo syringe. In addition, there are several subgingival adjuncts on the market. Though all show some value - I tried PerioChip, Atridox, and Arestin - I had the most success with Arestin. I use this product in pockets deeper than 5mm that are not responding well and continue to have high-risk bacteria on the microscope.
My dentist/employer prescribes systemic antibiotics when the infection is difficult to control. The combination of amoxicillin and metronidizole seem to be the most effective. Both are taken simultaneously, 500 mgs each, three times a day for seven days. We see the patient a month later to evaluate progress microscopically.
We occasionally send bacterial samples to the Microscopic Testing Laboratory at the University of Pennsylvania for detailed evaluations of organisms that cannot be detected on a live microscopic sample.
There is still much to learn, with many articles currently being published on periodontal microbiology, biofilms, irrigation, and anti-infective techniques. Strangely, with all the emphasis on periodontal infections, most studies still rely on probing and bleeding as the primary criteria of disease.
If periodontal diseases are infections, shouldn't we be trying to determine which patients are infected? In my experience, the microbiological status of the patient has been critical in the management of periodontal disease.
General health implications
After all these years of practicing anti-infective therapy, it's gratifying to finally see articles supporting what I've been teaching my patients. People are more aware of their dental health and how it pertains to them medically. Patients are interested in what they can do to stay healthy. My heart and diabetic patients are eager to help themselves because they know a healthy mouth is important to achieve a healthy body. New and current patients appreciate that I take their general health seriously.
An article in the October 2003 AARP magazine stated that periodontal disease is considered the second highest risk factor to heart attack and stroke behind smoking. AARP also published an article in March 2004 telling people to eliminate inflammation and infection in the mouth in order to preserve general health.
Another valuable use of the microscope is to determine whether gingival bleeding during probing and scaling is due to a periodontal infection or the use of blood thinners. Many patients who take daily aspirin tend to bleed more. If the bleeding is due solely to the effects of aspirin, there will be no increase in bacterial risk factors. No periodontal treatment is required, which might have been recommended if BOP was the determining criteria.
This is an exciting time to be a dental hygienist. We should no longer be called people who "clean teeth." The more people recognize the correlation between systemic diseases and their relations to oral health, the more impact we have as health care providers. I am proud to be a dental hygienist for 30 years. Good communication skills, a non-judgmental approach, patience and understanding help to interest, motivate, and succeed with patient care. The use of the microscope has been extremely instrumental in my success.
Sandy Sheffler, RDH, graduated from the Community College of Baltimore in 1973. She has been a clinical dental hygienist in private practice for 31 years. She can be contacted at [email protected].
Author's note: This article was written with input from Bill Landers, president of OraTec Corp., and Lynne H. Slim of Perio C Dent, Inc. The article is dedicated to Barry S. Buchman, DDS, who always looked past the conventional to do and see things before anyone else was willing to look.