Dental hygienists and an interprofessional approach to temporomandibular joint (TMJ) disorders
Temporomandibular joint disorders (TMD) should not be a foreign subject in the dental industry. First-year dental hygiene students are taught the anatomy and physiology of the head and neck, and they dive into the muscles of mastication. Additionally, they’re taught how the adjacent muscles and joints function through intraoral and extraoral assessments to ultimately recognize how dysfunctional movement of the jaw presents.
What is TMJ?
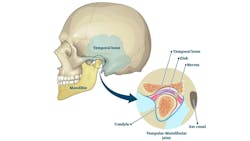
According to Johns Hopkins Medicine, TMJ is defined as two joints that connect the lower jaw to the skull. More specifically, they’re the joints that slide and rotate in front of each ear, and they consist of the mandible (the lower jaw) and the temporal bone (the side and base of the skull).1
What are TMDs?
According to Johns Hopkins Medicine, TMDs are disorders of the jaw muscles, temporomandibular joints, and the nerves associated with chronic facial pain. Any problem that prevents the complex system of muscles, bones, and joints from working together in harmony may result in a TMD.1
The National Institute of Dental and Craniofacial Research classifies TMD by the following: myofascial pain, internal derangement of the joint, and degenerative joint disease. Myofascial pain is considered the most common form of TMD. It results in discomfort or pain in the fascia and muscles that control jaw, neck, and shoulder function. Internal derangement of the joint occurs when the jaw is dislocated and there is a displaced disc or an injury to the condyle. Lastly, degenerative joint disease is when osteoarthritis or rheumatoid arthritis affects the jaw joint.1
Hygienists know many basics of TMJ
In dental hygiene school, we were taught the basics when it came to the symptoms of the jaw. We were able to recognize that if a patient presented with symptoms of potential TMD, we had the skills and knowledge to provide them with the utmost comfort throughout their dental hygiene appointment. As research develops, researchers are beginning to understand that TMD may be so much more than just “clicking of the jaw and/or bruxism with or without pain.”
In the article The Complexities of TMD, Stacia Ewing recognizes that TMD can no longer be considered easily treatable with fabrication of a mouthguard or splint. Researchers are finding that TMD is a multifaceted condition, and many studies are taking a more holistic approach to diagnosis and treatment.2
It’s important to understand that currently there isn’t enough research that shows manual therapy can be used as a treatment method to resolve TMD, however, a dental professional can collaborate with an RMT to help alleviate symptoms related to suspected TMD.
How other disciplines help with TMJ treatment
Registered massage therapists (RMTs) can play a significant role in the interdisciplinary treatment of TMDs, which involve a complex network of muscles, not just around the jaw, but extending to the neck, shoulders, and upper back. When these muscles become overactive, strained, weakened, or imbalanced, they contribute to the chronic pain and dysfunction many TMD patients experience.
Manual therapy is one of many techniques RMTs may use when trying to alleviate symptoms of TMD. Manual therapy and exercises are skills applied by clinicians that directly or indirectly target a variety of anatomical structures or systems that are used with the intent of creating beneficial changes in some aspect of the patient's pain experience.3
In TMD clients, manual therapy can reduce muscle tension, enhance the range of motion in the jaw, and alleviate any pain associated with TMD. RMTs may also incorporate, implement, and suggest intraoral massage, acupuncture, myofascial release, and trigger point therapy to their TMD clients as these are particularly effective in directly treating the muscles of mastication, giving patients improved jaw function and noticeable relief from pain.
As dental hygienists, we’re familiar with orofacial myofunctional therapy (OMT). When properly trained, we’re able to identify patients for disorders that may benefit from OMT. We understand that myofunctional therapy can improve oral and facial function by retraining the muscles. However, have you ever thought that an RMT can deliver this same care?
RMTs with myofunctional therapy training can also bring another dimension to TMD care by focusing on the functional patterns of breathing, swallowing, and tongue posture. Many people with TMD have chronic postural issues and hypermobility that can exacerbate their jaw problems. For example, a forward head posture or low tongue position can place additional strain on the TMJs. Exercises that strengthen and stabilize the tongue, jaw, and throat muscles can help reduce clenching, grinding, and improper swallowing. Restoring normal function and muscle balance may decrease the workload on the TMJs and reduce the frequency and intensity of TMD symptoms.
A patient’s TMD journey often starts with their dentist or dental hygienist, who can identify the dysfunction. Together, dental professionals and RMTs can provide patients with a cohesive treatment plan that addresses the mechanical, muscular, and functional components of TMD.
With open communication and shared expertise, the dental team and complementary health-care providers can provide multifaceted support for long-term relief and improved quality of life for TMD patients. Interprofessional collaboration is key to improving patient outcomes.
References
- Temporomandibular disorder (TMD). Johns Hopkins Medicine. August 8, 2021. Accessed November 16, 2024. https://www.hopkinsmedicine.org/health/conditions-and-diseases/temporomandibular-disorder-tmd
- Ewing SS. The complexities of TMD. RDH magazine. October 1, 2007. October 1, 2007. https://www.rdhmag.com/pathology/temporomandibular-joint-dysfunction/article/16407092/the-complexities-of-tmd
- Bishop MD, Torres-Cueco R, Gay CW, Lluch-Girbés E, Beneciuk JM, Bialosky JE. What effect can manual therapy have on a patient’s pain experience? 2015;5(6):455-464. doi:10.2217/pmt.15.39B
About the Author

Whitney Foster, RDH
Whitney Foster, RDH, has a demonstrated history of working in various roles in the dental field. In the last year, Whitney has been published in various publications within the industry and developed a continuing educational course that focused on interprofessional collaboration. With her passion for oral health care and the relationship to overall health, Whitney continues to support, mentor, and advocate on the subject for fellow dental hygienists.

Melissa Violette, RMT, OMT
Melissa Violette, RMT, OMT, is a clinic owner, educator, and entrepreneur. In May 2024, she opened Welland TMJ, a clinic dedicated to helping people conquer TMDs and OMDs. With a focus on rehabilitation, she uses manual therapies as well as myofunctional therapy to help patients overcome their symptoms.