Protecting patients with allergies to dental products
Perhaps you've heard the tragic story of an 11-year-old girl from California, named Denise Saldate, who died after being exposed to a prescription toothpaste that contained a milk-derived ingredient. Denise had a severe dairy allergy and her parents were unaware that the product contained milk proteins. As explained in Allergic Living, Denise’s parents had been accustomed to checking labels since she was a young child, but they did not examine the ingredient listing on this occasion.1 Since they had never seen milk listed as a toothpaste component before, they figured that it was safe for their daughter.
Denise’s dental office had prescribed the product after noticing several areas of decalcification on her teeth. The girl was excited to be using a new special toothpaste, but she tragically ended up experiencing a fast-moving anaphylactic reaction after applying the product. Denise ran to her mother immediately after she started brushing and told her that she was having an allergic reaction. The child’s mother used an Epipen as well as asthma inhaler, but neither managed to halt the anaphylactic reaction in time.
As a dental professional, I believe that we all can learn from this terrible tragedy. Allergies are all too common and we should be doing everything we can to prevent any reactions from occurring while patients are under our care. No one wants to think about anaphylactic shock occurring while they are working on a patient, but it is a real possibility. We need to be fully prepared at all times for any emergency situation that may happen in the dental office.
When thinking about allergies in the dental office, the focus is often placed on what medications a person is allergic to, such as penicillin or sulfa drugs. Knowing if a patient has a latex allergy is also stressed too. But other types of allergies, such as those to ingredients in commonly used dental products, can be just as important when it comes to keeping your patients safe. Do you feel like you are as prepared as you could be?
The basic science behind an allergic reaction
As explained by the American Academy of Allergy, Asthma, and Immunology, an allergic reaction occurs when an individual’s immune system overreacts to a harmless substance, which is referred to as an allergen.2 These substances can range from dust, pollen, certain foods, pet dander, insect bites to latex. The first time that a person is exposed to an allergen, it may not cause a reaction. However, after the person is sensitized, subsequent exposures to the allergen can produce an allergic reaction. In response to this perceived threat, the immune system triggers the production of special antibodies called immunoglobulin E (IgE). This leads to a cascade of events that results in symptoms manifesting in the nose, lungs, throat, sinuses, ears, and the lining of the stomach and skin.
As explained in Medscape, there are two basic types of hypersensitivity reactions that can occur from the use of dental products in patients with allergies3:
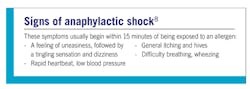
Type I (immediate hypersensitivity reaction): This type of reaction can be systemic or localized. It involves the release of histamine and other mediators from mast cells and basophils. Seasonal allergies are an example of this type of response and symptoms such as sneezing, runny nose, nasal congestion, and red eyes are typical. More severe reactions, such as anaphylactic shock also occur with this type of allergic reaction.
Type IV (cell-mediated immunity, delayed hypersensitivity reactions): This type of reaction can take 24-48 hours to develop, or sometimes longer. It is mediated by T cells instead of antibodies. A common example includes contact dermatitis that develops from exposure to poison ivy and nickel.
Being prepared while in the dental office
During a preventative appointment, have you ever had a patient ask if a dental product that you would be using contained a specific ingredient such as gluten or a red dye? Did you know the answer already when they asked? If not, were you able to look up the answer immediately? In the dental profession, it pays to be prepared as possible as time is always a factor and you want a patient to be confident in your abilities.
This preparedness starts with being familiar with all the products that you use on a regular basis. Many product websites do a thorough job of explaining whether they contain ingredients such as latex, gluten, or dyes that your patient may be sensitive to. An even better resource to utilize when allergies are a concern is the allergen ingredient and declaration statement that details all ingredients and possible allergens in a product. All dental product manufacturers are required to provide this documentation to dental offices upon request.
If you are unsure of whether a product contains a specific ingredient when a patient in your chair has a known allergy, it may be best to avoid use of the product altogether and seek out a suitable alternative. For example, if a patient has a sensitivity to red dye and you are not confident that your prophy paste does not contain this ingredient, use pumice to polish or a prophy angle that is paste free. Another great option would be to use an air polisher if your office has one.
Another key component to allergy preparedness is being extremely familiar with your patient’s medical history. As most dental professionals will agree, patients do not always tell us everything they need to when you update their medical history. Often, it is up to the hygienist to ask the right questions. For example, you can begin by asking a patient if he or she has ever had an allergic reaction to any substance. Then inquire as to what that specific reaction was. Sometimes when patients fill out medical history forms, they only list allergies to medications, not realizing that other types of allergies need to be disclosed too. Furthermore, it also helps to explain that you want to make sure that any products used during the appointment at any time are completely safe for them.
Being aware of the possible allergies in dental products is also a critical component of preparedness. According to a systemic review published in the Journal of Clinical and Diagnostic Research, the number of dental materials that may cause reactions are quite extensive.4 It includes amalgam, latex, sealant materials, sodium hypochlorite, titanium, nickel-chromium alloys, composites, local anesthesia, and impression materials. As this is the case, patients may not be aware of all the possible allergies that they may have. Watching for symptoms such as redness, itching, burning, or swelling is critical at all times. With dental materials, such as amalgams or composites, a delayed oral lichenoid-like reaction may occur directly adjacent to the restoration, so patients may call in at a later time to address this concern.
Addressing gluten sensitivity in patients
Gluten sensitivity is a common concern and the one that I most often get asked about by my patients. Celiac disease, an autoimmune disease in which the body’s reaction to gluten damages the small intestine, affects one out of a hundred people worldwide, according to the Celiac Disease Foundation.5 If a patient has a relative with Celiac disease, there is a 10% chance that they will also develop it. Furthermore, one percent of people with gluten sensitivity have a special type called refractory celiac disease which can be fatal. One eighth of a teaspoon of gluten is all it takes to damage the small intestine of someone who has this disease, so caution must be exercised with all dental products used in affected patients.
If you have any doubt with a dental product, don’t use it. The Celiac Disease Foundation website contains a helpful list of dental materials and oral care products that don't contain gluten.
Celiac disease: How dental professionals can help
Be cautious when using latex
One of the scariest facts about allergies is that they can develop at any point in a person’s life.6 I learned this lesson early on as a dental hygienist. In 2007, my office used latex gloves for the most part and reserved the nitrile ones for the patients with allergies. One day as I was working on a female patient in her forties, I noticed that her lips began to swell up and her face began to get red around the border of her mouth. I asked her if she had a latex allergy and she replied, “No.” I immediately notified the doctor and I was instructed to give the patient Benadryl to alleviate the symptoms. Additionally, I recommended that the patient be tested for a latex allergy, but she did not seem too concerned at the time.
Six months later, when the patient returned for her recare appointment, she disclosed that she had been hospitalized for anaphylactic shock a few months ago. The woman had been blowing up latex balloons at birthday party and ended up having a severe reaction. The patient had never followed through with the recommended testing since she had never had a problem with latex until recently. Thankfully, she fully recovered from the event, but the distressing part is that this health emergency could have been prevented. My office never used latex again after that.
Presently, it is common for most dental offices to no longer use latex gloves, but do you know what other types of products may still contain latex? Rubber dams are widely utilized in dentistry, as well as prophy cups, rubber stoppers, and mouth props, which all can contain latex.7 The nose bridge of the patient safety glasses is another item that may cause concern for those people with latex reactions. Even products you may recommend for home care, such as a rubber interdental pick, can cause latex reactions. So, although you can try to limit your patient’s latex exposure, it can be a challenge to avoid it completely.
In the dental profession, one of our main goals is to provide our patients with top notch oral care. Part of this effort involves meeting all your patients’ safety needs. Watching out for any type of allergic reaction and listening to your patients’ concerns is critical. The next time a patient tells you that they have an itch on their face during an appointment, make sure it is just a momentary discomfort and not an initial sign of a more serious allergic reaction.
Editor's note: This content was originally published in 2019 and has been updated as of April 2025.
References
1. Smith G. After daughter’s fatal reaction to toothpaste, mother calls for caution. Allergic Living website. https://www.allergicliving.com/2019/04/15/after-daughters-fatal-reaction-to-toothpaste-mother-calls-for-caution. Published April 15, 2019.
2. Allergic reaction definition. Academy of Allergy, Asthma, and Immunology website. https://www.aaaai.org/conditions-and-treatments/conditions-dictionary/allergic-reaction.
3. Buelow B, Routes JM. Immediate hypersensitivity reactions. Medscape website. https://emedicine.medscape.com/article/136217-overview. Updated February 9, 2015.
4. Syed M, Chopra R, Sachdev V. Allergic reactions to dental materials—a systematic review. J Clin Diagn Res. 2015;9(10):ZE04-ZE09. doi:10.7860/JCDR/2015/15640.6589.
5. Celiac Disease Foundation website. https://celiac.org/.
6. Donovan J. Adult-onset allergies. WebMD website. https://www.webmd.com/allergies/features/adult-onset-allergies#1.
7. Guidelines to promote safe practice in the dental environment for latex allergic patients. Australian Society for Clinical Immunology and Allergy website. https://www.allergy.org.au/hp/papers/management-of-latex-allergic-patients/the-dental-environment. Published March 2010.
8. Delves PJ. Anaphylactic reactions. Merck Manual Consumer Version website. https://www.merckmanuals.com/home/immune-disorders/allergic-reactions-and-other-hypersensitivity-disorders/anaphylactic-reactions. Revised January 2018.
About the Author

Amber Metro-Sanchez, BA, RDH
Amber Metro-Sanchez, BA, RDH, practices dental hygiene with Chris Bible, DDS, at Comfort Dental in Fort Wayne, Indiana. She also works as a professional educator on behalf of Waterpik. Amber was a member of the 2015 Colgate Oral Health Advisory Board. She is also a contributing author for the Colgate Professional and Colgate Oral Care Center webpages. Reach her at [email protected].