It's no surprise to dental professionals that a healthy mouth is critical to overall health and wellness. But could a healthy mouth also lead to healthier eyes? Emerging research suggests that infection and inflammation may travel between the mouth and the eyes. Dental hygienists are poised to offer valuable education and prevention regarding oral health and eye health, including potential vision problems and blindness.
With the infectious pathway, bacteria travel from the oral cavity and metastasize to the eye. The eye, just like the mouth, skin, and gut, has a unique and individualized microbiome. Factors that may influence the makeup of the eye microbiome include ethnicity, geographic region, age, contact use, and oral and intestinal health.1
Harmful pathogens can enter the bloodstream and lymphatic system and travel throughout the body to the eye. Dysbiosis can occur when bacteria, viruses, fungi, and parasites disrupt the normal eye microbiome. Eye diseases are more likely to emerge when the microbiome is out of balance. Some examples of eye diseases associated with nonocular microbes include dry eye syndrome, keratitis, blepharitis, and conjunctivitis. High bacterial loads in the oral and intestinal parts of the body, including Bacteroides and Prevotella, have been implicated in an altered eye microbiome.2
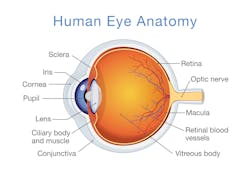
In 2017, a study published in the Journal of Glaucoma concluded that poor oral health, an altered oral microbiome, and the number of missing teeth all may be considered risk factors for glaucoma pathology.3 With all types of glaucoma, the optic nerve in the back of the eye that connects the eye to the brain is damaged (figure 1). With the inflammatory pathway, the highly vascular supporting periodontal structures around the teeth become injured by harmful periodontal bacteria. The host inflammatory response is triggered. Chemicals in the form of histamine, bradykinin, and prostaglandins are released by the damaged cells. This results in tissue swelling caused by the chemicals leaking into the surrounding blood vessels. The inflammatory cascade is marked by inflammation throughout the body, which increases pressure around the eye. Increased pressure in the eye irritates or damages the optic nerve. In the June 2021 issue of Investigative Ophthalmology & Visual Science, research corroborated previous scientific studies regarding the association between poor oral health and primary open-angle glaucoma (POAG).4
Further reading: Jenn's vision: Victim of eye injury turns into advocate for eyewear for dental patients
Glaucoma is classified as a progressive optic nerve disease. POAG is the most common form of glaucoma and makes up approximately 90% of all cases. Glaucoma is one of the leading causes of blindness for people over the age of 60. Glaucoma may have no symptoms in its earliest stages, and 50% of people with the condition may not even know they have it.5 POAG may have no symptoms other than a slow loss of peripheral or central vision.
The theory that oral bacteria enter the bloodstream and travel to other parts of the body, with the potential to create systemic inflammation, has been discussed since the late 1800s.8 Now, we know that harmful oral pathogens have been linked to a wide range of conditions—including diabetes, obesity, certain cancers, cardiovascular disease, and much more.
Dental hygienists can be empowered to play a key role in health coaching for optimal oral and eye health. Here are some key strategies that can be incorporated into routine dental visits:
- Ask about and encourage routine eye examinations during the medical history review, including social and family history.
- Raise awareness by discussing the various oral-systemic links, including the mouth-eye connection.
- Assess oral health at every visit. Prevention of oral infections and eye diseases is ideal. If they are not prevented, early detection is key.
- Promote a healthy lifestyle for risk reduction, including tobacco cessation, nutritional counseling, breathing, weight management, and sun protection for the head, neck, lips, and eyes.9
- Provide effective biofilm removal during professional cleanings and consider the use of lasers,10 ultrasonics,11 and guided biofilm therapy.12
- Recommend evidenced-based biofilm removal techniques for home care, such as WaterPik13 and PerioProtect trays.14
Dental hygienists are essential primary care providers who are highly qualified to provide education on emerging oral-systemic connections. An altered oral microbiome may not only affect the teeth and gums but also vision and eye health.
Editor's note: This article appeared in the April 2022 print edition of RDH magazine. Dental hygienists in North America are eligible for a complimentary print subscription. Sign up here.
References
- St. Leger T. Meet the eye microbiome. Scientific American. June 23, 2019. Accessed January 31, 2022. https://www.scientificamerican.com/article/meet-the-eye-microbiome/
- Napolitano P, Filippelli M, Davinelli S, Bartollino S, dell’Omo R, Costagliola C. Influence of gut microbiota on eye diseases: an overview. Ann Med. 2021;53(1):750-761. doi:10.1080/07853890.2021.1925150
- Polla D, Astafurov K, Hawy E, Hyman L, Hou W, Danias J. A pilot study to evaluate the oral microbiome and dental health in primary open-angle glaucoma. J Glaucoma. 2017;26(4):320-327. doi:10.1097/IJG.0000000000000465
- Coggins K, Husain A, Parsegian K, Whitson JT. Association between poor oral health and risk of glaucoma. Invest Ophthalmol Vis Sci. 2021;62(8):1605.
- Glaucoma. Symptoms and causes. Mayo Clinic. Accessed January 15, 2022. https://www.mayoclinic.org/diseases-conditions/glaucoma/symptoms-causes/syc-20372839
- Glaucoma. Eyes and vision conditions. American Optometric Association. Accessed January 10, 2022. https://www.aoa.org/healthy-eyes/eye-and-vision-conditions/glaucoma
- Baiu I, Melendez E. Periorbital and orbital cellulitis. JAMA. 2020;323(2):196. doi:10.1001/jama.2019.18211
- Akshata KR, Ranganath V, Nichani AS. Thesis, antithesis, and synthesis in periodontal and systemic interlink. J Indian Soc Periodontol. 2012;16(2):168-173. doi:10.4103/0972-124X.99257
- Tips to prevent vision loss. Centers for Disease Control and Prevention. Reviewed August 10, 2021. Accessed January 31, 2022. https://www.cdc.gov/visionhealth/risk/tips.htm
- Convissar RA. Principles and Practice of Laser Dentistry. Mosby; 2011.
- Vyas N, Wang QX, Manmi KA, Sammons RL, Kuehne SA, Walmsley AD. How does ultrasonic cavitation remove dental bacterial biofilm? Ultrason Sonochem. 2020;67:105112. doi:10.1016/j.ultsonch.2020.105112
- Drago L, Del Fabbro M, Bortolin M, Vassena C, De Vecchi E, Taschieri S. Biofilm removal and antimicrobial activity of two different air-polishing powders: an in vitro study. J Periodontol. 2014;85(11):e363-e369. doi:10.1902/jop.2014.140134
- Gorur A, Lyle DM, Schaudinn C, Costerton JW. Biofilm removal with a dental water jet. Compend Contin Educ Dent. 2009;30(Spec No 1):1-6.
- Keller D. How to manage oral biofilm using PerioProtect as a minimally invasive method for lasting oral health. Dental Products Report. 2010;44(7):54-55. Accessed January 31, 2022. https://providers.perioprotect.com/wp-content/uploads/2020/01/DPRO-HowToManage-Perio.pdf