The brain’s security system: Helping dental patients protect their blood-brain barrier
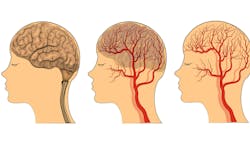
The blood-brain barrier (BBB) is a security system for the brain. It’s a protective layer of tightly packed cells that lines the blood vessels in the brain, preventing harmful substances such as toxins, bacteria, and viruses from getting in while allowing essential nutrients and oxygen to pass through.
Think of the BBB as a highly selective filter that keeps the brain safe from infections and inflammation. If it becomes weakened or leaky, harmful substances can sneak in, leading to brain inflammation and damage. This is especially concerning in conditions such as Alzheimer's and vascular dementia, where a compromised BBB may allow an inflow of neurotoxic blood-derived debris, cells, microbial pathogens, or inflammatory molecules to reach the brain and accelerate cognitive decline. Maintaining a healthy BBB is key for brain function and long-term neurological health.
Important proteins and BBB disturbances
Claudin-5 is an endothelial-specific protein that’s located predominantly in blood vessels, especially in the brain. It is integral to the formation of tight junctions between endothelial cells, thereby fortifying the BBB. As the most prevalent tight junction protein, claudin-5 functions as a seal to control the passage of molecules between the bloodstream and brain tissue. A reduction or compromise in claudin-5 levels results in increased permeability of the BBB, which permits undesirable substances to penetrate brain tissue. High blood pressure, diabetes, stroke, and chronic inflammation can weaken claudin-5 and reduce BBB function.
Porphyromonas gingivalis, one of the red complex pathogens, can compromise the integrity of the BBB, potentially facilitating the onset and progression of neurodegenerative diseases. Bacteremia induced by P. gingivalis not only increases BBB permeability and allows harmful substances to infiltrate brain tissues, but also compromises the secretion of virulence factors such as gingipains and lipopolysaccharides (LPS).1
These factors contribute to the degradation of tight junction proteins, including claudin-5.2 P. gingivalis operates comprehensively by moving from periodontal pockets into the bloodstream, circulating throughout the body and eventually translocating. This pathogen releases inflammatory mediators and degrades proteins, leading to dysfunction of the BBB. This aligns with 3,000 years of history that indicate the oral influence, particularly periodontitis, on the general health of humans.3
Pathologic states including trauma, hypoxia, infection, activation of the clotting system, inflammation, and environmental toxins can cause BBB disturbances.4 Chronic inflammation, specifically the inflammatory markers IL-6, TNFɑ, and proinflammatory cytokines, break down the tight junction between the barrier cells and make it more permeable.5
Intermittent hypoxia (IH) and sleep fragmentation is the direct result of obstructive sleep apnea (OSA). OSA patients exhibit increased BBB permeability due to systemic inflammation, oxidative stress, and changes in cerebral blood flow due to IH.6,7 Uncontrolled hypertension can change the ultrastructure of endothelial cells in cerebral arterioles, leading to BBB leakage. Studies have found that individuals with high blood pressure show greater leakage, indicating a direct relationship between blood pressure levels and BBB integrity.8,9
The role of dental providers in BBB prevention
Dental providers measure blood pressure during visits and can assist patients by referring them to appropriate specialists or discussing strategies to lower blood pressure. There is a significant association between periodontal disease and elevated blood pressure. Individuals with periodontitis are more likely to experience high arterial blood pressure and possess a 30% to 70% increased likelihood of also having hypertension.10
Do periodontal treatments work? There are positive findings that nonsurgical periodontal therapy can be effective in lowering blood pressure in patients with prehypertension and periodontitis.11 A randomized controlled trial in 2017 demonstrated that intensive periodontal intervention may be an effective means of lowering blood pressure and endothelial microparticles (EMP) in patients with prehypertension and periodontitis.12
EMPs are small vesicles released from endothelial cells due to stimuli such as inflammation, injury, and stress. Their activation can promote blood clotting, damage blood vessels, disrupt BBB tight junctions, and increase oxidative stress molecules, which further harms the barrier.13 Oxidative stress—the imbalance between the production of reactive oxygen species (ROS) and the body's ability to detoxify—can damage cellular components such as DNA proteins and lipids and lead to various diseases.
Oral dysbiosis triggers inflammation, which can lead to an increase of ROS and oxidative stress.14 Type 2 diabetes (T2DM) and elevated blood sugar can affect the BBB and its surrounding blood vessels. Diabetes can cause damage to endothelial cells, disrupt pericytes (cells that wrap around blood vessels to stabilize the barrier), and impair astrocytes (which provide nutrients to neurons and regulate BBB permeability).
Additionally, diabetes can activate microglia cells (the brain's immune cells) and lead to an inflammatory response that may affect the BBB. Diabetes also increases the production of ROS, promotes inflammation, and causes changes in transport proteins, impacting nutrient supply and waste removal in the brain.15 Oral medicine providers can help T2DM patients by not only reducing inflammation, but improving glycemic control.16
Let’s applaud the value of providers, yet again. They provide blood pressure surveillance, guidance, and lowering; sleep disordered breathing assessment and treatment; periodontal pathogen identification and elimination; and metabolic disorder improvement, which all impact the BBB and cognitive health. All in a day’s work for oral health-care providers.
References
1. Lei S, Li J, Yu J. et al. Porphyromonas gingivalis bacteremia increases the permeability of the blood-brain barrier via the Mfsd2a/Caveolin-1 mediated transcytosis pathway. Int J Oral Sci. 2023;15:3. doi.org/10.1038/s41368-022-00215-y
2. Salhi L, Al Taep Y, Salmon E, Van Hede D, Lambert F. How periodontitis or periodontal bacteria can influence Alzheimer’s disease features: a systematic review of pre-clinical atudies. J Alzheimer’s Dis. 2023;96(3):979-1010. doi:10.3233/JAD-230478
3. Seymour GJ, Ford PJ, Cullinan MP, Leishman S, Yamazaki K. Relationship between periodontal infections and systemic disease. Clin Microbiol Infect. 2007;13 Suppl 4:3-10. doi:10.1111/j.1469-0691.2007.01798.x
4. Shlosberg D, Benifla M, Kaufer D, Friedman A. Blood-brain barrier breakdown as a therapeutic target in traumatic brain injury. Nat Rev Neurol. 2010;6:393-403. doi.org/10.1038/nrneurol.2010.74
5. Kadry H, Noorani B Cucullo L. A blood–brain barrier overview on structure, function, impairment, and biomarkers of integrity. Fluids Barriers CNS. 2020;17:69. doi.org/10.1186/s12987-020-00230-3
6. Gagnon K, Baril AA, Gagnon JF, et al. Cognitive impairment in obstructive sleep apnea. Pathol Biol (Paris). 2014;62(5):233-240. doi:10.1016/j.patbio.2014.05.015
7. Zolotoff C, Bertoletti L, Gozal D, et al. Obstructive sleep apnea, hypercoagulability, and the blood-brain barrier. J Clin Med. 2021;10(14):3099. doi:10.3390/jcm10143099
8. Santisteban MM, Ahn SJ, Lane D, et al. Endothelium-macrophage crosstalk mediates blood-brain barrier dysfunction in hypertension. Hypertension. 2020;76(3):795-807. doi:10.1161/HYPERTENSIONAHA.120.15581
9. van den Kerkhof M, de Jong JJA, Voorter PHM, et al. Blood-brain barrier integrity decreases with higher blood pressure: A 7T DCE-MRI study. Hypertension. 2024;81(10):2162-2172. doi:10.1161/HYPERTENSIONAHA.123.22617
10. Muñoz Aguilera E, Suvan J, Orlandi M, Miró Catalina Q, Nart J, D'Aiuto F. Association between periodontitis and blood pressure highlighted in systemically healthy individuals: results from a nested case-control study. Hypertension. 2021;77(5):1765-1774. doi:10.1161/HYPERTENSIONAHA.120.16790
11. Lanau N, Mareque-Bueno J, Zabalza M. Impact of nonsurgical periodontal treatment on blood pressure: a prospective cohort study. Eur J Dent. 2024;18(2):517-525. doi:10.1055/s-0043-1772246
12. Zhou QB, Xia WH, Ren J, et al. Effect of intensive periodontal therapy on blood pressure and endothelial microparticles in patients with prehypertension and periodontitis: a randomized controlled trial. J Periodontol. 2017;88(8):711-722. doi:10.1902/jop.2017.160447
13. Lehner C, Gehwolf R, Tempfer H, et al. Oxidative stress and blood-brain barrier dysfunction under particular consideration of matrix metalloproteinases. Antioxid Redox Signal. 2011;15(5):1305-1323. doi:10.1089/ars.2011.3923
14. Shang J, Liu H, Zheng Y, Zhang Z. Role of oxidative stress in the relationship between periodontitis and systemic diseases. Front Physiol. 2023;14:1210449. doi:10.3389/fphys.2023.1210449
15. Li X, Cai Y, Zhang Z, Zhou J. Glial and vascular cell regulation of the blood-brain barrier in diabetes. Diabetes Metab J. 2022;46(2):222-238. doi:10.4093/dmj.2021.0146
16. Simpson TC, Clarkson JE, Worthington HV, et al. Treatment of periodontitis for glycaemic control in people with diabetes mellitus. Cochrane Database Syst Rev. 2022;4(4):CD004714. doi:10.1002/14651858.CD004714.pub4
About the Author

Anne O. Rice, BS, RDH, CDP, FAAOSH
Anne O. Rice, BS, RDH, CDP, FAAOSH, founded Oral Systemic Seminars after over 35 years of clinical practice and is passionate about educating the community on modifiable risk factors for dementia and their relationship to dentistry. She is a certified dementia practitioner, a longevity specialist, a fellow with AAOSH, and has consulted for Weill Cornell Alzheimer’s Prevention Clinic, FAU, and Atria Institute. Reach out to Anne at anneorice.com.