A 27-year-old male visited a dental office for a checkup and prophy. Radiographic examination revealed a radiolucency around the apex of tooth #24.
History
When questioned about the area, the patient admitted to a history of trauma to the area a couple of years earlier. He remarked that the area was not painful. The patient appeared to be in a good general state of health and was taking no medications at the time of the dental appointment.
Examinations
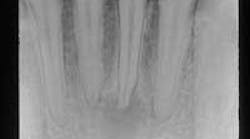
Examination of the head and neck region revealed no palpable lymph nodes. All vital signs were found to be within normal limits. Oral examination revealed no soft tissue or bony abnormalities. Radiographic examination re-vealed a well-defined radiolucency around the apex of tooth #24 (see film). The mandibular anterior teeth were tested for vitality; teeth #22, 23, 25, 26, and 27 all tested vital while tooth #24 tested nonvital.
Clinical diagnosis
Based on the clinical information presented, which of the following is the most likely diagnosis?
• radicular cyst
• parulis
• periapical scar
• periapical cemental dysplasia
• residual cyst
Diagnosis
• radicular cyst
Discussion
The radicular cyst (also known as periapical cyst or apical periodontal cyst) is, by far, the most common cyst identified in the jaw. More than 50 percent of all periapical radiolucent lesions are radicular cysts.
Periapical radiolucent lesions such as the radicular cyst - as well as the periapical granuloma and periapical abscess - all result from pulpal death and necrosis. The most frequent cause of pulpal death and necrosis is dental caries. Trauma may also be a cause. With pulpal necrosis, an inflammatory process is seen that extends from the pulp chamber and canals to the periapical region of the affected tooth. The lesion that results may present in an acute form as an abscess or, in chronic form, as a granuloma.
The periapical granuloma is an accumulation of chronically inflamed granulation tissue seen at the apex of a nonvital tooth. The radicular cyst is a lesion that develops over a prolonged period of time within an existing periapical granuloma.
A cyst, by definition, has an epithelial lining. The epithelial lining of the radicular cyst is derived from the epithelial rests of Malassez found within the periodontal ligament.
Clinical features
The radicular cyst most often occurs in the third through sixth decades. The radicular cyst may also affect deciduous teeth. Most radicular cysts occur in the maxilla; the anterior regions are involved more commonly than the posterior regions.
Most radicular cysts are asymptomatic and present no clinical signs or symptoms. The affected tooth is seldom painful.
The radicular cyst is usually discovered during routine radiographic examination. The radicular cyst is always associated with a nonvital tooth. Electric pulp testing can be used to determine pulp vitality.
It is impossible to diagnose a radicular cyst from a radiograph alone. Although impractical, histologic examination of the periapical tissue is needed to make a definitive diagnosis.
There are no distinctive radiographic differences between a radicular cyst, a periapical granuloma, and a periapical abscess. The size and appearance of the borders (corticated vs. noncorticated) are not diagnostic. The typical periapical cyst appears as a round to ovoid radiolucency. The size may range from less than 1/2 centimeter to several centimeters in diameter. The borders may be corticated or noncorticated. Root resorption may be seen.
When interpreting radiographs, it is important to remember that the radiographic appearance of periapical inflammatory lesions cannot be used to distinguish between the different forms of periapical disease. Unless a definitive diagnosis via biopsy is obtained, the dental professional may describe what is seen as a "periapical radiolucency" or "apical periodontitis."
Diagnosis
Although impractical and not routinely performed for a periapical lesion, histologic examination is necessary to make a definitive diagnosis of a radicular cyst. The histologic appearance of a radicular cyst is that of a true cyst with an epithelial lining; the cyst lining is comprised of stratified squamous epithelium and varies in thickness. The cyst wall is made up of fibrous connective tissue that often exhibits an inflammatory cell infiltrate.
Treatment
There are two treatment options for all periapical inflammatory lesions (radicular cyst, periapical granuloma, periapical abscess): extraction and curettage of the apical lesion or endodontic therapy. Large lesions may need to be treated with endodontic therapy combined with a biopsy or marsupialization, decompression, or fenestration. As with all periapical inflammatory lesions, post-treatment radiographs at one- and two-year intervals are strongly advised in order to rule out lesion enlargement and verify healing.
If the periapical inflammatory lesion does not resolve, then endodontic retreatment may be an option. Periapical surgery is also an option but is often reserved for lesions that measure greater than two centimeters in diameter. Periapical surgery may include excision and biopsy of the lesion, removal of the apical portion of the root, and sealing the foramen of the canal. A radicular cyst or other periapical inflammatory lesion that is adequately treated does not recur.
Joen Iannucci Haring, DDS, MS, is an associate professor of clinical dentistry, Section of Primary Care, The Ohio State University College of Dentistry.