Winning the battle against sensitivity
By Mary Govoni, CDA, RDH, MBA
A frequent complaint that dental hygienists hear from patients is tooth sensitivity in areas where there is exposed dentin. This sensitivity is primarily due to hypersensitive dentin that is exposed to various triggers in the oral cavity. It may be localized to a few teeth or generalized throughout the patient’s mouth. Causes of the dentin hypersensitivity may be due to temperature changes, or exposure to other stimuli, such as chemicals (acids, for example).
Hygienists are constantly challenged with researching products and techniques to offer as solutions to their patients with dentin hypersensitivity. It is important to understand the biomechanics and causes of hypersensitivity to better recommend optimal treatment and/or home care products for each patient.
This is especially important because new products for treating hypersensitivity are introduced frequently.
Researchers have defined dentin hypersensitivity as “short, sharp pain arising from exposed dentin in response to stimuli typically thermal, evaporative, tactile, osmotic or chemical and which cannot be ascribed to any other form of dentinal defect or pathology.”1,2 Common sites for hypersensitive dentin are the cervical and root areas on teeth, where dentin is exposed by loss of enamel due to erosion, abrasion, attrition or abfraction.
Dentin exposure may also be caused by gingival recession, due to toothbrush abrasion, periodontal disease, surgery to reduce periodontal pockets, or crown lengthening procedures. When these conditions are present, the protective covering over the dentinal tubules, the smear layer, is removed and the openings to the dentinal tubules are exposed to stimuli in the oral cavity. When the dentinal tubules are open, fluid is able to move within the tubules and stimulates the nerve receptors on the junction between the dentin and pulp (see Figure 1, courtesy of Tokuyama Dental America). Research has demonstrated that the wider the dentinal tubules, the greater the fluid movement, and thus greater sensitivity results.3,4
Exposed dentin is not only a cause of painful sensitivity to patients; it is also prone to caries. Thus, clinical researchers have worked extensively to develop products and modalities to prevent dentinal hypersensitivity from occurring and from progressing.
It is important to note, however, that not all hypersensitivity is due to exposed dentin. Patients may experience sensitivity due to other clinical factors, such as cracked teeth, caries, whitening procedures, bruxism, and other factors. Hypersensitivity due to exposed dentin is typically diagnosed by blowing a stream of air onto the suspected area or touching the suspected area with an explorer, using a lateral motion on the tooth structure.
Once the other causative factors for sensitivity have been eliminated, and a diagnosis has been made, treatment modalities for dentin hypersensitivity can be evaluated by the dentist and hygienist. Factors influencing treatment and product choice may include the amount of exposed dentin, the degree of sensitivity, tooth brushing habits, and overall oral hygiene of the patient. In addition, if dentin hypersensitivity is due to tooth brushing or other patient habits, continuing those habits will negatively affect treatment success.
Types of dentin desensitizers
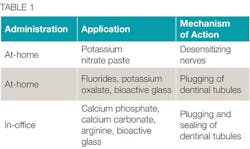
Many treatment modalities and products are available to hygienists for protecting exposed dentin and relieving patients’ hypersensitivity. The treatments are categorized by the method of application or mode of administration - either at-home or in-office treatments. Table 1 lists the common classes of treatments available for hygienists to recommend, dispense, and/or apply on patients with exposed dentin.
When researching products, it is critical for the hygienist to verify what the product is intended for, how it is applied, and whether an at-home application should be combined with an in-office product. Since the patient symptomology and sensitivity may vary, it may be beneficial to have a variety or combination of treatments to offer patients.
Treatment may include home use of toothpastes containing potassium nitrate, adhesive strips containing potassium oxalate, fluoride rinses and pastes, and combinations of fluoride and calcium and phosphate (Recaldent, for example) or calcium phosphosilicate bioactive glass (NovaMin, for example).
These products may be available over the counter, or as prescription products dispensed in the practice or at the pharmacy. Many of these products decrease sensitivity as well as promote remineralization of tooth structure. At-home treatments are most commonly recommended for patients with sensitivity that is generalized throughout the mouth.
In-office treatments include application of fluoride and fluoride varnish, use of polishing pastes with arginine, as well as a variety of resins. The in-office treatments are more commonly used for patients with localized areas of hypersensitivity and tend to have a longer lasting effect on the sensitivity, with bioactive glasses and resins having the longest effectiveness. A combination of products - at-home and in-office - may be indicated for some patients.
Other considerations
While hygienists are dedicated to providing their patients with the most effective treatment options for hypersensitivity, many factors influence product selection.
These factors include ease of application, long-term effectiveness, compatibility with tissue and existing restorations, and cost to the patient. Patient compliance or noncompliance with at-home products may factor into recommended treatment and suggested products. If the patient’s sensitivity is caused by toothbrush abrasion, recommendations should be given for less damaging techniques and devices.
As stated before, a combination of products may be indicated for some patients, such as a take-home product used in conjunction with an in-office treatment. If making this recommendation to the patient, the hygienist must be aware of product compatibility and any potential contraindications for combining the chemistries of the products.
The manufacturer’s instructions for use (IFUs) should be the first thing that a hygienist reviews when selecting a product and prior to using a product for the first time. IFUs contain valuable information that will affect the successful use of a product and improve outcomes for patients.
Although there are CDT codes for application of desensitizers, as we well know, many benefit plans do not cover the procedure. The hygienist and other members of the dental team must be well versed in presenting treatment options, including the benefit to the patients and help those patients to value the treatment and the relief that they may have from use or application of desensitizing products.
Ongoing relief
Yet another factor in determining which product is best suited for a particular patient is the length of time that the relief may last. A great deal of success has been achieved with long-term use of sensitivity toothpastes that desensitize the nerve endings in the dentinal tubules, but it may take days or weeks of using the pastes for the patient to get relief (and continued use of the toothpaste is indicated).
Products that block or plug the dentinal tubules typically provide more immediate and longer-lasting relief. These include bioactive glass ionomer resins such as Activa from Pulpdent, as well as paint-on resins such as Pain-Free Gel from Parkell and Shield Force Plus from Tokuyama.
For example, Tokuyama’s product information states that its Double Block Technology provides instant comfort for patients that can last up to three years, safeguarding them from additional pain in the future. Shield Force Plus is also glutaraldehyde free, making it a safer and more convenient treatment option than some other products.
Figure 2 offers an example of the application instructions for the treatment of dentinal hypersensitivity/coating of exposed cervical dentin using Shield Force Plus by Tokuyama Dental America, an in-office treatment option for long-term desensitizing.
Again, hygienists should be thorough in their product research to compare product characteristics, such as the ability of a resin applied to exposed dentin to penetrate the dentin for optimal occlusion of dental tubules as well as retention on the tooth.
Treating dentin hypersensitivity is a good news/bad news situation. The good news is that there are many effective products to choose from in the current marketplace. The bad news (if you call it that) is that it does take some time to sort through the products, the information for application in various situations and patients, and determine the appropriate protocol for each individual patient. RDH
Mary Govoni, MBA, RDH, CDA, RDA, is an internationally recognized speaker, author, and consultant, working with dental teams for more than 40 years on clinical efficiency, infection prevention, ergonomics, and team communication. She has published numerous articles in Dental Economics, The Dental Assistant Journal, RDH magazine, Dentistry Today, Inside Dentistry, and others.
References
1. Holland GR, Narhi MN, Addy M, Gangarosa L, Orchardson R. Guidelines for the Design and Conduct of Clinical Trials on Dentine Hypersensitivity. Journal of Clinical Periodontology, 1997;24:808-13.
2. Orchardson R, Collins W. Clinical Features of Hypersensitive Teeth British Dental Journal, 1987; 162,252-256.
3. Absi EG, Addy M, Adams D. Dentin Hypersensitivity: A Study of the Patency of Dentinal Tubules in Sensitive and Non-Sensitive Cervical Dental. Journal of Clinical Periodontoloty. 1987;14:280-4.
4. Rimondini L. Baron C, Carrassi A. Ultrastructure of Hypersensitive and Non-Sensitive Dentin. Journal of Clinical Periodontology. 1995; 22:899-902.