Perfectly placed, perfectly sealed: 10 best practices in dental sealant application
Dental caries remains a critical public health crisis, affecting more than 2.4 billion adults and 520 million children worldwide.1 This underscores the urgent need for proven preventive solutions such as dental sealants. Dental sealants penetrate the pits and fissures of occlusal surfaces and function by effectively forming a physical barrier that inhibits the colonization of microorganisms while creating a favorable surface to help patients maintain better oral hygiene.
Sealant materials are primarily categorized into resin-based sealants (RBS), glass ionomer sealants (GI), and polyacid-modified resin sealants. RBS, widely used in clinical practice, may include fluoride-releasing components.2 GI sealants release fluoride over time, are moisture-tolerant, and easy to place, while resin-modified versions enhance durability and reduce moisture sensitivity.2
Polyacid-modified resin sealants combine the adhesive and fluoride-releasing properties of GI with the strength of RBS, offering easier application, especially for young or uncooperative patients.2 Here, I’ll focus on discussing resin-based sealants due to their prevalence and clinical application.
Proficiency in sealant placement
I talked with a colleague who has nearly 30 years of clinical experience, and we discussed a significant concern. She explained that while she was once trained to apply sealants, her current focus on periodontal and implant care has caused her to lose the proficiency to place sealants effectively.
I remember being instructed to read a chapter from a textbook on sealants and then immediately apply my knowledge by placing sealants on a patient. This approach lacked sufficient guidance and led to challenges achieving proper retention with my sealants. With additional hands-on practice and education, I was able to develop the skills to perform the procedure effectively.
This situation underscores the broader challenge of skill retention among dental hygienists when certain techniques are not regularly practiced. It highlights the critical importance of comprehensive training, hands-on experience, and ongoing professional development to maintain and enhance proficiency in essential preventive procedures such as dental sealant application.
Given the current state of oral health care, in which dental caries persists as a common disease worldwide, revisiting the topic of sealants feels especially urgent. Add the growing number of patients seeking nonfluoride interventions and the possibility of fluoride being removed from water sources in the future, it’s clear that dental hygienists must be equipped to respond to an anticipated rise in caries rates. As one of the most effective preventive measures available, dental sealants are an indispensable tool to meet this challenge.
Challenges and concerns
However, there remain barriers and misconceptions surrounding the use of sealants. Misunderstandings about proper application techniques, uncertainty about which teeth to seal, and skepticism toward materials all contribute to their underutilization in clinical settings. For example, parents may express concerns about BPA exposure from sealants in their children, despite a wealth of evidence proving these fears are unwarranted. Research highlights that the minute amount of BPA exposure from sealants is far less than what one might encounter through everyday activities.3
That said, clinicians can alleviate these concerns by selecting sealant materials free of BPA. Beyond these misconceptions, the ADA underscores the multifaceted benefits of sealants. Not only do they serve as primary prevention for caries, but they can also halt the progression of early, noncavitated caries when applied correctly.3 Additionally, many dental plans cover sealants under CDT code 1351, often extending coverage to adolescents and adults.3 This presents a valuable opportunity for patients to invest in their oral health while reaping the long-term cost savings of avoiding restorative treatment for preventable caries lesions.
Filled or unfilled?
While the advantages of sealants are well-documented, there’s still some uncertainty among dental hygienists about technical aspects of their use, such as understanding the term “fill rate” in relation to resin-based sealants. Sealant products differ in forms, viscosities, colors, and filler contents, which influence their physical properties, flowability, and wear resistance. Retention, crucial for sealant longevity, is theoretically enhanced in unfilled or low-filled sealants due to their low viscosity, allowing deeper fissure penetration.4
These sealants also save time and cost as they require no occlusal adjustments, wearing down quickly in the absence of fillers. However, incorporating fillers improves wear resistance and reduces shrinkage, contributing to greater durability and long-term effectiveness.4 Grandio Seal by Voco is a nano-fissure sealant with a filler content exceeding 70% w/w, offering high abrasion resistance and durability, even under the stress of daily mastication. It has thixotropic properties that allow the material to flow easily under pressure, ensuring thorough and bubble-free penetration into the deepest fissures and stabilizing once the pressure is released for precise application.
A 2022 systematic review and meta-analysis found no significant difference in retention rate or caries development between filled and unfilled resin-based sealants within a two-year follow-up.4 The choice of sealant should be individualized based on factors such as fissure type, patient age, and habits.4
Reflecting on these insights, it’s evident that proper training and ongoing education are critical to ensure dental hygienists are well prepared to apply sealants with confidence. We must also make it a point to educate ourselves and our patients about evidence-based guidelines for sealant use. This proactive approach equips us to dispel myths, offer sound preventive solutions, and position our patients for optimal oral health in the long term.
To address the challenges associated with skill retention and to ensure long-term proficiency in dental sealant application, here are 10 comprehensive steps designed to promote effective retention and consistent application techniques.
10 steps for successful dental sealant placement
1. Train staff: Train the clinical team on sealant placement through hands-on sessions with extracted teeth or typodonts, addressing issues such as contamination, curing errors, and incomplete preparation to reduce mistakes and improve sealant retention.5
2. Assemble your armamentarium: To ensure successful placement of the dental sealant and a smooth and efficient procedure, assembling the appropriate armamentarium is key. Materials include isolation materials (gauze, cotton rolls, rubber dams), a curing light, sealant material, acid etch gel, a mouth mirror, explorer, prophy brush, cotton pellets, and articulating paper (figure 1).
3. Prepare the tooth surface
Mechanical debridement (traditional): Use an air polisher or pumice slurry to eliminate plaque and debris for better retention. These methods remain effective for preparing the enamel, yet evidence shows advancements in chemical cleaning for superior bacteria removal that leads to better retention.6
Chemical debridement: One drop of over-the-counter 3.5% hydrogen peroxide penetrates deep into grooves, removing plaque and killing bacteria. This can be applied by using a cotton swab or microbrush.2 Combining or selecting the appropriate cleaning method ensures a clean surface and optimal sealant adhesion.6
4. Identify and address residual caries: Examine grooves carefully after cleaning for any signs of caries. Based on its staining effect, applying a small amount of silver diamine fluoride (SDF) may help detect carious lesions.5
5. Establish effective moisture control: Moisture control is essential for successful sealant placement, as saliva contamination can lead to increased microleakage and reduced bond strength.
6. Apply acid etching: A systematic review and meta-analysis determined that dental sealants applied with phosphoric acid etching exhibit significantly lower microleakage, establishing this method as superior to alternatives such as air abrasion and laser conditioning.1 Acid etching, particularly using 37% phosphoric acid, remains the gold standard for effective tooth surface preparation. Research comparing etching times of 15, 30, 45, and 60 seconds found that a 60-second etching duration resulted in the highest shear bond strength.1 However, the marginal difference between 30 and 60 seconds suggests that a 30-second etching time can still provide clinically acceptable outcomes.1
7. Remove excess moisture (optional): An optional technique for improving sealant retention involves removing residual moisture from grooves using a "water chaser" or prime-and-dry material. This method can enhance outcomes by effectively displacing water and ensuring a clean, dry enamel surface.6
8. Maintain a dry, uncontaminated field: Continuously monitor isolation and dryness, addressing contamination promptly with re-etching and drying.
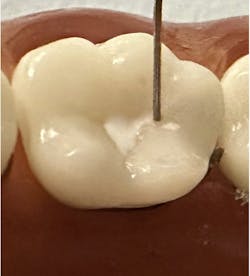
9. Use precise application techniques: Apply the sealant material with precision, ensuring it penetrates deep pits and fissures. Use an explorer to manipulate the material into hard-to-reach areas. Avoid leaving excess material, which can interfere with occlusion or lead to premature wear.
10. Properly light cure: Use a curing light with verified output strength (minimum 1,000 mW/cm²) for adequate polymerization.5 Place the light close to and perpendicular to the sealant surface. Follow the manufacturer’s curing time recommendation for optimal results and inspect for any uncured material.
3 considerations for dental sealant placement
1. Hypomineralized teeth: Hypomineralized teeth exhibit increased resistance to etching due to their reduced microporosity compared to normal teeth following acid etching.7 To ensure optimal retention, establish adequate micropores on the enamel surface. In cases of enamel hypomineralization, etch times may need to be extended to achieve the necessary level of microporosity.7
2. Fluoride before sealant placement: Avoid using fluoridated prophy paste or applying fluoride varnish before placing a dental sealant. Fluoride can hinder the etching process by reducing the enamel's ability to form the microporous texture essential for optimal sealant retention. This is due to the formation of fluorapatite layers, which are more resistant to acid and less responsive to etching.
3. Cannulas and placement techniques: Voco's Grandio Seal features ultrafine placement cannulas, allowing precise application into deep pits and fissures with minimal need for additional manipulation (figure 2).
By contrast, other brands often use large, blunt-ended cannulas that cannot effectively penetrate intricate grooves. These large tips typically require the use of an explorer to guide the material as their blunt profile cannot match the tapered design of an explorer for accessing fine details.7 (figure 3).
By adhering to these considerations, dental professionals can optimize their sealant application techniques and outcomes. Proper selection of materials and tools, coupled with meticulous attention to technical details, ensures reliable and durable preventive care for patients. As the oral health-care landscape evolves, dental sealants remain an indispensable component of our tool kit, and it’s our responsibility as practitioners to use them effectively.
Editor's note: This article appeared in the March 2025 print edition of RDH magazine. Dental hygienists in North America are eligible for a complimentary print subscription. Sign up here.
References
1. Ng TC-H, Chu C-H, Yu OY. A concise review of dental sealants in caries management. Front Oral Health. 2023;17(4):1180405. doi:10.3389/froh.2023.1180405
2. Eagle IT. Encouraging sealant use. Dimens Dent Hyg. February 26, 2021. https://dimensionsofdentalhygiene.com/article/encouraging-sealant-use/
3. Dental sealants. American Dental Association. Accessed December 7, 2024. https://www.ada.org/resources/ada-library/oral-health-topics/dental-sealants
4. Bagheri E, Sarraf AS, Shekofteh K. Comparison of the success rate of filled and unfilled resin-based fissure sealants: a systematic review and meta-analysis. Front Dent. 2022;8(19):10. doi:10.18502/fid.v19i10.8855
5. Christensen GJ. Why are sealants failing? Dent Econ. June 1, 2021. https://www.dentaleconomics.com/science-tech/article/14202168/why-are-dental-sealants-failing
6. Van Haywood B, Capehart KL, Cooper JR. Strategies to ensure successful sealant placement. Dimens Dent Hyg. February 7, 2020. https://www.dimensionsofdentalhygiene.com/article/strategies-ensure-successful-sealant-placement/
7. Arcaro J. 6 reasons why sealants fail. Today's RDH. April 19, 2022. https://www.todaysrdh.com/6-reasons-why-sealants-fail/
About the Author

Joy D. Void-Holmes, DHSc, BSDH, RDH
Joy D. Void-Holmes, DHSc, BSDH, RDH, a leader in oral health-care with nearly 30 years of experience, excels in dental education and hands-on workshops. Founder of Dr. Joy, RDH, and JELL-ED, she champions self-care, personal boundaries, and cutting-edge clinical techniques. With degrees from Howard, Maryland, and Nova Southeastern, Dr. Joy shapes the future of dental hygiene as a consultant examiner, board member, and advocate for innovation and professional growth.