Risk assessments: Integrating intraprofessional health models
Dorothy Garlough, MPA, RDH
A respected chiropractor in my community was at yoga this morning. Knowing that she had moved her chiropractic practice to a new location six months ago, I asked her how she liked her new location. She lit up with excitement, and without a nanosecond of hesitation said she loved it. She felt that the move had elevated the care of her patients. You see, her office had moved to a health facility that had a physician, a pharmacist, a hearing specialist, a physiotherapist, and a massage therapist all in the same building. She expanded on the benefits of this holistic model, revealing that the proximity to other health-care providers offered her the ability to consult about the needs of her patients and design care in a holistic manner. I listened intently and noted that, as of yet, there was no dental professional in the building.
The model of multiprofessional health-care providers in the same location stems from the growing recognition that the systems of the human body are interconnected. What is diseased in one region often displays symptoms somewhere else. We are whole beings, after all, not just a back, a heart, or a mouth. Consulting with other health professionals only makes sense.
Change is occurring. One forward-looking group, the Wellness Dentistry Network (wellnessdentistrynetwork.com), is developing “whole” health dentistry. Leading organizations such as the Mayo Clinic say that the mouth is the window to the health of the body.1 Many others, including myself, have written on the inflammation connection of periodontal diseases and the diseased body.2
Today I want you to consider the possibilities of what could be. I want you to imagine how dentistry could and should be part of an intraprofessional dialogue about the care of people within society. If the mouth is the window to the body, dental professionals need to be sitting across the table from other practitioners and contributing to the overall care of patients.
RISK ASSESSMENTS AND TODAY’s HEALTH CARE
What information do we need to take part in “person-centered” care? In my view, one critical component is the risk assessment. Thorough risk assessments are what enable health professionals to estimate the likelihood that certain events (such as oral disease) will occur. Traditionally, dental hygienists have gathered this kind of information by recording medical histories, taking bleeding scores, measuring periodontal pockets, examining attachment loss, looking at wear, evaluating for caries, noting extractions, performing oral cancer screenings, etc. But with goal-oriented, person-centered care, more information is required. Health providers need to assess not only the functional needs of patients, but also their cognitive levels.
In addition, more complete risk assessments record vital signs, evaluate systemic conditions, note disabilities, review behavioral risk, and record dietary needs. Implementing these types of risk assessments in dental practices helps flag conditions early and enables timely referrals to other health-care providers that could be life-saving.
With this kind of risk assessment, handwritten charting begins to look like chicken scratch. Charts are so messy that they are nearly impossible to read. However, today we can use technology not only to keep data in order, but to run algorithms. Technology has evolved so that evidence-based algorithms now review the entirety of the data to assess risk. Personalized reports then help clinicians get a better handle on what risks are for patients. Data also offer clinicians entry points for conversations with patients. For example, personalized reports can help highlight needs for proceeding with treatment plans. Educating patients in this way not only influences them to comply with recommended treatment, but more importantly, it helps secure commitment in the first place.
Companies are producing different kinds of software to amalgamate large amounts of patient information. Three that I am familiar with are Colgate,3 Phillips Care,4 and PreViser.5
With the detail of the risk assessment, it is recommended to schedule an hour for the initial recording of the data. After that, it is simply a matter of recording changes at follow-up appointments.
The World Health Organization recognizes dental hygienists as primary health-care providers whose mandate is to help improve the quality of life of patients.6 It is estimated that by 2050, 20% of the population in the United States will be over the age of 65, with the vast amount of increase before 2030.7 The Centers for Disease Control and Prevention predicts that 70.1% of older citizens will have periodontal disease, leading to dental hygienists being even more broadly recognized as primary health-care providers.8
Developing collaborative links between health professionals to assess overall health is a trend worth promoting. Working with medical doctors, social workers, pharmacists, nutritionists, nurse practitioners, community health workers, ophthalmologists, etc., is the missing link in our health-care system. Developing collaborative competencies will go a long way in delivering person-centered care.
Collaborative competencies
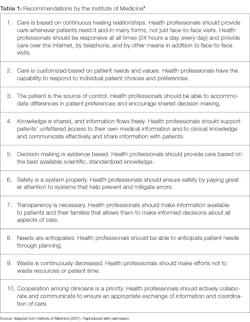
The guidelines in Table 1 are offered by the National Academies of Sciences, Engineering, and Medicine. They suggest how intraprofessional collaborative competencies need to intersect.9
As dental health professionals exercising collaborative competencies with intraprofessional treatment planning, our role is to identify oral-systemic associations that impact the diagnoses of patient outcomes. Dental professionals make their oral diagnoses and recommendations based on the following principles:
• Ongoing review of patients’ goals and treatment plans
• Active coordination between all health-care and supportive-service providers
• Ongoing open communication and information providing
• Education and training for providers
• Education and training for patients and, when appropriate, those important to them
• Performance measurement and quality input using feedback from the person and caregiver
• Time for discussions for an approach that considers medical conditions, functional abilities, and social supports that are ultimately guided by individual goals, dignity, and choice
• Providing evidence to ensure that patients are aware of their potential future disease states if no interventions occur
• Clinician recommendations and treatment plans guided by individualized care
It is my belief that we are on the cusp of change, where whole health will be the focus and dental professionals will be recognized widely as primary health-care providers. Technology will help us get there. Yet technology can do more. Wouldn’t it be wonderful if software could be developed that records patients’ medications (and other supplements they ingest) and offers contraindications, side effects, reactive properties, and genetic factors that could have effects? Algorithms could compile the information and offer contraindications with the push of a button. Perhaps software could also record findings in the emerging field of diagnosing saliva and look for bacterial or viral infections.
The future is pregnant with possibility! When all health-care specialties communicate broadly and openly, we will be practicing holistically. I realize I may not know of all the wondrous mashups of different models that exist. I invite my readers to fertilize the concept with other models they may know of, or simply share your wild ideas of what you can imagine. In the meantime, I will broadcast the benefits of having a dental professional in our community’s health park!
References are available in the online version of this article. Visit rdhmag.com and search for the title of this article.
Dorothy Garlough, MPA, RDH, is an innovation architect, facilitating strategy sessions and forums to orchestrate change within dentistry. As an international speaker and writer, Garlough trains others to broaden their skill sets to include creativity, collaborative innovation, and forward-thinking. She recognizes that engagement is the outcome when the mechanisms are put in place to drive new innovations. Connect with her at [email protected] or visit engagingteams.com.