by Nancy Burkhart, RDH, EdD
Notes and findings: The patient is a 51-year-old white female maintenance patient who has not had a dental appointment in over two years. She scheduled an appointment because a large growth is noticeable in the anterior region of her mouth, and this lesion has her concerned. The patient reports that the growth has been there for over one year and has grown considerably during that time. As the oral tissues are assessed, it is noted that the large lesion in the anterior is firm, smooth, and sessile (broad-based). The patient reports no pain, but does report that the growth can become somewhat ulcerated if she brushes too hard or traumatizes the area (see Figure 1).
Diagnosis: Peripheral odontogenic ossifying fibroma
Etiology: Peripheral odontogenic ossifying fibromas are reactionary lesions thought to originate from submucosal connective tissue and the periodontal ligament. The lesions are often confused with either the more vascular (red to pink) pyogenic granuloma, or the fibroma that demonstrates more tissue colored lesions. It is thought that an exuberance of tissue is caused by an initiating factor such as calculus, or a food particle such as a popcorn hull, that becomes lodged in the sulcus, creating an initial irritation.
Peripheral odontogenic ossifying fibromas occur more often in females and can be anywhere from 1.0 to 2.0 cm in size. They occur most often in young adults, originate from the periodontal ligament, and occur exclusively on the gingiva as a sessile or pedunculated mass. Peripheral odontogenic ossifying fibromas are classified most often in literature as reactionary lesions rather than neoplasms.
Figure 1
Neoplasms and infections may exhibit similar charactistics and must be considered in a differential diagnosis as well. Most localized gingival overgrowths are categorized into the following types of lesions seen clinically.
- Neoplasms
- Infections
- Fibromas
- Peripheral ossifying fibromas
- Pyogenic granulomas
- Giant cell granulomas
Method of transmission: The peripheral ossifying odontogenic fibroma is a reactionary type lesion, posing no contagion issues.
Pathogenesis Chronic irritation causes an abundance of fibrous connective tissue containing immature bone. Often patients traumatize the area again, and this promotes a cycle of more exuberant tissue formation and varying surface ulceration. There is a close resemblance to the pyogenic granuloma. It has been speculated that the peripheral ossifying odontogenic fibroma may be a latent type of pyogenic granuloma that has matured and developed bone. The lighter surface color is due to hyperkeratosis produced through trauma.
Perioral and intraoral characteristics: The lesions are normally found on the attached gingiva. The abundance of tissue is usually the same color as the surrounding tissue, with a smooth surface. Sometimes the surface may be more textured, depending upon the existing oral forces and location in the patient’s mouth. Additionally, the surface epithelium may be more of a dark color depending upon the amount of trauma and inflammation that is produced with the lesion.
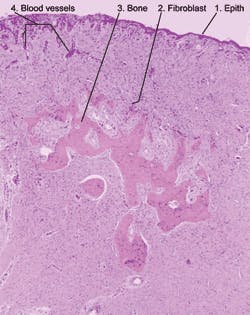
Figure 2
Distinguishing characteristics: Peripheral ossifying fibromas may appear similar to other soft tissue lesions and entities such as the pyogenic granuloma and the peripheral giant cell granuloma. Pyogenic granulomas may become more fibrous in appearance as they age, resembling the clinical charactistics of a peripheral ossifying fibroma. Normally, the pyogenic granuloma will appear dark pink to red, but they tend to become more “fibrotic” and lighter in color as they age. The importance of histological diagnosis becomes essential in differentiation of the lesions.
Significant microscopic features: Microscopically, the tissue is composed primarily of cellular fibroblasts with various types of calcification including bone, cementum and dystrophic calcification. The surface epithelium may exhibit varying degrees of ulceration (see Figure 2).
In the slide, the following areas are identified:
- Surface epithelium
- All small blue dot-like cells are nuclei of the lesion’s cells, fibroblasts
- Bone
- Dilated blood vessels due to the inflammation within the lesion
Treatment and prognosis: The treatment of choice is excision of the lesion with the periodontal ligament, and no recurrence is expected in most instances. Complete removal is indicated since peripheral odontogenic ossifying fibromas can reoccur when they are not adequately removed. It is advised that the lesion be removed down to the periosteum and that the adjacent teeth be scaled to remove any remaining irritants. This will assist in lowering the rate of recurrence (Neville, et al. 1995).
About the Author
Nancy Burkhart, RDH, EdD, is an adjunct associate professor in the Department of Periodontics at Baylor College of Dentistry and Texas A & M Health Science Center in Dallas. Nancy is also a co-host of the International Oral Lichen Planus Support Group through Baylor (www.bcd.tamhsc.edu/lichen). She is the co-author of General and Oral Pathology for Dental Hygienists, published by Lippincott Williams & Wilkins in Baltimore, which will be released in October 2007. She can be contacted at [email protected].
References
1. Buduneli E, Buduneli N, Unal T. Long-term follow-up of peripheral ossifying fibroma: report of three cases. Periodontal Clin Investig. 2001; 23(1): 11-14.
2. Eisen D, Lynch DP. The Mouth: Diagnosis and Treatment. Mosby; 1998. St. Louis, Mo.
3. Feller L, Buskin A, Raubenheimer EJ. Cemento-ossifying fibroma: case report and review of the literature. J Int Acad Periodontol. 2004 Oct; 6(4): 131-135.
4. Neville BW, Damm DD, Allen CM, et al. Oral & Maxillofacial Pathology. 2nd Ed. W.B. Saunders Company, Philadelphia, PA. 1995.
5. Regazi JA, Sciubba JJ, Jordan RCK. Oral Pathology: Clinical Pathologic Correlations. Saunders St. Louis, Mo. 2003.
6. Wright JM. Oral and maxillofacial pathology case of the month. Peripheral odontogenic (ossifying) fibroma. Tex Dent J. 2000 Nov. 117(11): 62, 69.