by Nancy Burkhart, RDH, EdD
Presentation: Mr. Sheraton, a 49-year-old male, is the patient. During the routine maintenance appointment, you notice a large area on the patient’s tongue that concerns you. Mr. Sheraton tells you that he has noticed the area as well when he brushes his tongue, but adds that it is not causing him much discomfort. Occasionally, he does notice a slight burning sensation when he eats his favorite spicy salsa.
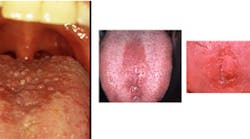
Notes and findings: The tongue appears to have a white coating that is thicker in some areas than others and is slightly fissured. You also notice that the filiform papillae appear denuded in the central portion. Additionally, you note that the tissue within the central part of the tongue has a smooth, pink appearance as well, with the darker pink areas forming an oval shape (Figure 1).
Clinical impressions: Since you have not encountered this before, you sort through many possibilities, and you question the patient about recent illnesses, changes in the use of dental products, foods, and lifestyle factors. Since you just attended a course on oral cancer and oral pathology, you have oral cancer as your primary differential diagnosis (this is not a bad thought until proven otherwise!). However, after sorting through the possibilities, some other areas of pathology begin to surface.
Diagnosis: Median rhomboid glossitis
Figure 2 depicts a median rhomboid glossitis in the center part of the tongue forming rhomboid shaped lesions.
Etiology and pathogenesis: Median rhomboid glossitis (MRG), also referred to as central papillary atrophy, was once thought to be a developmental defect that occurred during embryogenesis, caused by the failure of the tuberculum impar to be covered completely by the lateral processes of the tongue. MRG is found anterior to the circumvallate papillae. Since MRG is not found in children (Baughman, 1971) (Ugar-Cankal et al. 2005), a developmental etiology has been largely discounted; however, a direct cause has not been established.
Papillary atrophy is characteristic in MRG. The rhombus-shaped, well-demarcated, and central denuded area of the tongue exhibits a red to dark pink appearance. Studies and reports suggest that infection with C. albicans may be the causative factor. Wright (1978) in a review of the literature dating back to 1907, reported on the association of MRG with candida in 28 cases examined for fungal hyphae, thus linking candida to MRG. Similar lesions are found in the hard palate in relation to MRG, and the lesion has been called a “kissing lesion”(Allen, 1992) (Brown & Krakow, 1996).
MRG is also described as a form of hyperplastic candidiasis and the term median rhomboid glossitis is used when these lesions are found on the central portion of the tongue (Figure 2a). MRG candidiasis may cause the central portion of the dorsum of the tongue to lose filiform papillae.
MRG can be varied and is sometimes not clearly diagnostic to the clinician. Hyperplastic candidiasis may be present in other areas of the mouth as well, such as the commissures and the hard and soft palate. Associations with actinomyces have been proposed as well (Nowak & Szyfter, 2005).
Chronic candida infection can produce a hyperplastic type of tissue response. Whitaker and Singh (1996) suggested that - by the very nature of candida and its need for a warm, protected environment - the tongue provides a site conducive to candida overgrowth with the lingual papillae perhaps protecting the organisms. In this shielded environment, the organisms are protected from the normal cleansing and antibacterial effects of saliva, allowing the candida to flourish.
Another interesting theory involves the position of the tongue in relationship to the palate in speaking, swallowing, and the pressure applied during normal tongue movement. The relationship of the tongue to the palate is unique in each individual and the amount of time the two tissues are in contact would depend upon the structure, shape, tongue movements, and force of the tongue. Kessler (1996) suggested that perhaps some patients with MRG exert excessive pressure in the production of certain sounds such as “g,” “k,” and “j.” This pressure, in turn, might account for the nodularity sometimes found in relation to MRG (Figure 2b).
Oral candidiasis can exhibit other signs and symptoms as well. Lesions at the lip commissures exhibit a crusted, ulcerative appearance, and the terms angular cheilitis or perlèche are used. Candida also thrives under full and partial dentures (denture sore mouth), since the protective environment of the denture allows candida to become established.
Since candidal infections are opportunistic in nature, the presence of lesions such as MRG or hyperplastic candidiasis should raise the level of suspicion that the affected patient may have a compromised immune system. In fact, there is some evidence that both chronic hyperplastic candidiasis and MRG are seen more frequently in patients with HIV infection (Kolokotronis et al., 1994).
Method of transmission: MRG is not transmitted from one individual to another; however, candida can be transmitted from one person to another when the uninfected individual is susceptible or is in a low resistance state.
Approximately one-half of the general population carries candida in the oral cavity as a normal component of the microbial flora. The organisms become proliferative when local or systemic host resistance is reduced.
Perioral and intraoral characteristics: MRG has acquired its name because of the distinct features associated with the lesion. It is found in the central portion of the posterior dorsum of the tongue, classically exhibits a rhomboid-type shape and microscopically demonstrates an inflammatory process with embedded candidal hyphae. The clinical appearance is sometimes varied because of the amount and type of candida in the area, as well as perhaps other factors. The lesions can be raised, fissured, or lobulated and on occasion exhibit a darker color.
Distinguishing characteristics: MRG is found on the posterior and central portion of the dorsum of the tongue and has a rhomboid or diamond shape. The lesion may have a flat, darker pink, denuded appearance. Sometimes, because of the fact that some individuals may have a diffuse, white coating on the tongue, the appearance of MRG may have a varied appearance.
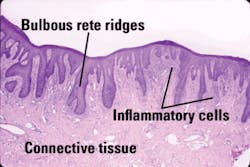
Significant microscopic features: The clinical appearance is important in MRG diagnosis, and the more information the clinician can provide to the oral pathologist, the more certain an accurate diagnosis will be made. The pathologist will base the diagnosis on the bulbous, elongated epithelial rete ridges that produce a psoriasis-like pattern, loss of the lingual papillae, parakeratosis of the epithelium, and inflammation (Figure 3). The most important diagnostic clue is the presence of candidal hyphae in the superficial epithelium (Figure 4). Providing a photograph of the clinical appearance of the lesion is another tool to assist the pathologist in an accurate diagnosis.
Differential diagnosis: Candida infection, chemical burns, syphilis patches depending upon the clinical appearance, geographic tongue, nutritional deficiencies, lichen planus, and traumatic ulcerations would be considerations. With any unexplained lesion, oral cancer is always considered, although the center of the tongue is not a common area for malignancy.
Treatment: The patient is treated with an antifungal regimen, including replacement of the toothbrush, and any other oral device that may cause reinfection by the organism. A careful evaluation of the systemic health of the individual is needed with a possible referral to a physician.
Antifungals that are commonly used include nystatin, clotrimazole, fluconazole and ketoconazole. Since the candidal hyphae are embedded in the tissue, some authorities believe that the use of systemic antifungal agents is the most effective treatment. The antifungals aid in diminishing the candida, but the appearance of MRG may or may not diminish clinically.
If the patient is a denture wearer, as with the treatment of any type of candida, the appliances, dentures, or any other oral devices should be treated with antifungal agents.
Digital photography is utilized in most offices today, and this is a great opportunity to document lesions to note future changes and to assist in a diagnosis. Subtle changes are more readily detected with digital photography, and images are used to compare the growth of lesions, decrease in size of lesions, and color changes. With any unusual type of entity or lesion, changes do occur sometimes and any unusual findings should be evaluated anew. RDH
Nancy Burkhart, RDH, EdD, is an adjunct associate professor in the Department of Periodontics at Baylor College of Dentistry, Texas A & M Health Science Center in Dallas. Nancy is also a co-host of the International Oral Lichen Planus Support Group through Baylor (www.bcd.tamhsc.edu/lichen). She can be contacted at [email protected].
References
Allen CM. Diagnosing and managing oral candidiasis. J Am Dent Assoc 1992;23:77-82.
Baughman RA. Median rhomboid glossitis: a developmental anomaly? Oral Surg 1971; 31:, 56-65.
Brown RS, Krakow AM. Median rhomboid glossitis and a “kissing” lesion of the palate. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996: Nov; 82(5):472-3.
Kessler HP. Letter to the editor-Median rhomboid glossitis. Oral Surg Oral Med Oral Pathol Oral Edod. 1996 Oct;82(4):360.
Kolokotronis A, Kioses V, Antoniades D, Mandraveli K, Doutsos I, Papanayotou P. Median rhomboid glossitis. An oral manifestation in patients infected with HIV. Oral Surg Oral Med Oral Pathol. 1994; 78:36-40.
Nowak K, Szyfter W. Median rhomboid glossitis-change of inflammation origin or developmental anomaly? Otolaryngol Pol. 2005; 59(6):857-60.
Nowak K, Szyfter W. Median rhomboid glossitis-change of inflammation origin or developmental anomaly? Otolaryngol Pol. 2005; 59(6):857-60.
Regezi JA, Sciubba JJ, Jordan R. Oral Pathology: Clinical Pathological Correlations. Saunders, St. Louis, 2003.
Terai J, Shimahara M. Atrophic tongue associated with candida. J Oral Pathol Med. 2005 Aug; 34(7): 97-400.
Ugar-cankal D, Denizci S, Hocaoglu T. Prevalence of tongue lesions among Turkish schoolchildren. Saudi Med J. 2005 Dec; 26(12):1962-7. Whitaker SB, Singh BB. Letter to the editor:Cause of median rhomboid glossitis. Oral surg Oral Med Oral Pathol Oral Edod. 1996 April;81(4):379-80.Wright, BA. Median rhomboid glossitis: Not a misnomer. Oral Surg Oral Med Oral Pathol. 46:6: 1978:806-14.