Goals and Strategies for Successful Patient Compliance
by Lois N. Dryer, RDH, MS
Communication skills are learned early. Toddlers point to what they want and make noises, and eventually sound out and repeat words they hear from older siblings and adults. As their vocabulary increases, words are linked together to create sentences. By age two they understand and follow the rules of communication as defined by their culture or social group.
Communicating does not happen only verbally. Other forms are visual, written, and nonverbal, such as body language or dress. Whatever form it takes, its purpose is the same; to concisely deliver a specific message. But to be effective, the message must not only be delivered but also received and understood.
People communicate by using symbols to represent feelings, ideas, and objects. But because symbols are arbitrary, they are not necessarily intrinsically connected to what they represent. For example, "apple" no longer refers solely to a fruit. Words can also be ambiguous and therefore open to individual interpretation. For people who are not communicating in their native language, idioms may prove very challenging. What words mean has a direct connection to the relationship of those communicating. Diverse cultural, social and hierarchal status can obscure the meaning of verbal symbols.
Effective communication between the oral health care provider and patient has a number of goals. First, patients need to understand and accept how their habits, behaviors, and general health impact their oral health status. Second, they must understand what professional and personal treatment options are available. Third, they must comprehend and commit to all aspects of the agreed upon treatment plan.
Successful oral health home care education involves patients. Including patients in the analysis of their intake data gives the hygienist an opportunity to invite them into all aspects of their dental hygiene care and establish rapport. An empathetic inquiry that discerns a patient's concerns also helps individualize the treatment and create a team approach to the care plan. It's here that the art of active listening is highlighted. By paraphrasing, verifying consequences, and preparing to listen, the hygienist is able to ensure that what the patient says is what he or she really means.
When paraphrasing, the listener repeats in his or her own words what the speaker said. This allows the listener to make sure that what was said was valid, and to focus and remember key points. The hygienist can verify the patient's statements by adding details to the original statement: "Was the difficulty you reported with flossing specific to the front teeth?" Communication free of distractions creates an environment that supports conversation.1
Barriers to effective communication are environmental and attitudinal. Loud or inappropriate music, office and other operator noises, and pain are factors that can derail conversation. A patient's personal problems, illness, perception of low value of the treatment, prior negative experiences (fear), and relationships with staff all present barriers to the treatment message.2
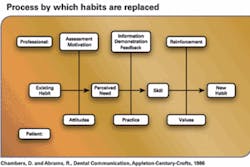
Once patients acknowledge their role in their health status, the discussion of an oral hygiene home care plan can begin. When it comes to teaching home care skills, hygienists know they are not starting with a blank slate. Both the adult and child patient come to us with some level of dexterity and understanding of home care. It is their misunderstanding of the process that results in challenges.
When instructing children it is advisable to do so within the context of the family. Due to limited psychomotor and cognitive skills, a family member may need to help a child with oral home care. Children under the age of eight lack sufficient motor skill to be successful brushers and flossers. They are also unable to adequately respond to assessment questions concerning their health histories, habits, and behaviors. Adults, with their greater dexterity and experience, present different challenges. Regardless of age or the need for a caretaker, the communication factors are the same.
As communicators, hygienists must be authentic and credible. Patients have to see their providers as caring and invested in their clients' well–being and success. Hygienists should strive to present a professional image through their appearance, demeanor, speech, knowledge, and expertise. Helping patients learn should be the focus of the process. It is the job of the hygienist to support patients' knowledge by recognizing their strengths and weaknesses, and sharing information tailored to their individual needs.3
Adults bring to the learning process the sum of their prior experiences. Established home care habits are in place because patients believe the habits work for them. This is true even in cases of neglect or error. Teaching strategies that rely on fear tactics, "show and tell," and external motivators that promise to fix the problem don't work.1 Patients are willing, motivated, and ready to learn and comply when the information is viewed as an asset that will address a need or desire.
Because adults view themselves as independent and capable, it is important that the communication process respect their beliefs, attitudes, and successes. Establishing a setting that allows patients to express their concerns, fears, and wishes eliminates barriers to learning. By including the patient in all aspects of the process, from assessment and planning to implementation and evaluation, the learner's self–esteem is preserved and the learning process becomes a shared process. If the new or modified skill can be linked to an established skill or notion, all the better!
Assessment includes documentation and analysis of both verbal and nonverbal communication. Fifty–five percent of our communication is nonverbal. Posture, eye contact, facial expressions, and gestures can substitute for words.
They amplify, modify, and control communication, many times unconsciously. The hygienist should be sensitive to these cues as they are sometimes more real than words. By matching a patient's words to his or her actions, the hygienist can check whether or not the message is valid. The patient who clutches the armrest when telling the provider that all is well is sending a mixed message.2
Planning a home care regimen together assures that both the patient and hygienist are on the same page. Objectives, priorities, choice of materials, teaching methods, short and long–term goals, and self evaluation strategies are articulated so that when instruction is implemented there is no confusion. It's easy for the oral care provider to forget how difficult learning a new psychomotor skill can be. To make it easier, it's helpful to break down complex information into smaller parts. Allow for individual pacing, as some patients perform faster than others. Provide immediate feedback and positive reinforcement. If possible, create a mental image of the psychomotor skill to help translate the task into a neuromuscular action.
Compliance depends on the interaction of patient and professional. Success breeds success. The methods and techniques of communication the dental hygienist uses are central to success. Half of all patients forget or misunderstand some part of home care instruction within one week of an appointment. However, this statistic decreases if patients take responsibility for their care and feel that their health–care provider attended to their needs and concerns.1 Successful instruction and patient compliance are a result of effective communication.
References
1. Chambers D, Abrams R. Dental Communication, Appleton–Century–Crofts, 1986.
2. Glasscoe D. "Creating Communication Excellence," www.professionaldentalmgmt.com.
3. Petersen M. "Treating Adult Patients as Partners in Dental Health Education," Dental Hygiene, August 1986.
4. Daniel S, Harfst S. Mosby's Dental Hygiene Concepts, Cases and Competencies, Mosby, 2002.
5. Petersen M. "Dental Hygienists as Adult Educators," Access Magazine, Sept–Oct, 1995.
About the Author
Lois N. Dreyer, RDH, MS, is an associate professor in the Department of Dental Hygiene, New York City College of Technology.