Most dental hygienists want to provide excellent care, so much so that they are often willing to endure discomfort or work long hours. For these practitioners, everything is worth it as long as they know patients are getting the best possible care. This is why the clinical effects of dull instruments are, for many hygienists, the most alarming of their consequences, even though the others, such as occupational pain, are no less important overall.
In previous articles covering the results of our State of Sharpening Survey, we’ve discussed how dull instruments can hurt a practice’s bottom line, even though many employers discourage sharpening or delay replacing instruments in a misguided attempt to save money. We’ve also covered how hygienists can improve or refresh sharpening technique to help make sharpening less stressful and time consuming. The damage that dull instruments do to a practice’s bottom line comes in many forms. Perhaps a patient complains to her family and friends about how a hygienist struggled to scale her teeth.1 Perhaps another develops periodontal issues despite having diligently taken care of his teeth, and leaves the practice in frustration.2 Perhaps appointments take longer and so the practice sees fewer patients.2
As with most issues in the dental practice, the clinical aspect can never be fully separated from the bottom line (despite some less-than-ethical employers’ attempts to do so). The instrument-
patient-clinician relationship is an important one in the dental practice, and is significantly damaged when instruments aren’t optimally maintained. Dull instruments not only hurt the health of the patient, but also of the practitioner.
Risks to patients
In addition to making calculus removal downright difficult, dull instruments can burnish the surface of calculus, “leaving deposits for microbes to inhabit,” wrote Dianne Watterson, MBA, BS, RDH, in a 2012 RDH article.3
“Calculus attaches by mechanically interlocking to the crystals of the tooth, using the acquired pellicle. Burnished calculus is a subgingival deposit that has had its outermost layer shaved off—but not fully removed—so that the surface is smooth yet still attached to the tooth surface, contributing to disease . . . These areas of burnished deposits will contribute to persistent gingival inflammation and bleeding, in addition to providing a constant food source for more bacteria,” wrote sharpening expert Tami Wanless.4
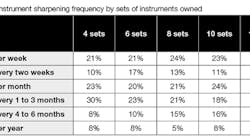
Commenting on the survey results (table 1), Tim Irwin, a vice president at Nordent Instruments who has been involved with continuing education about sharpening for two decades, said that “Hygienists need sharp instruments to deliver quality care for two reasons. First, sharp instruments provide the clinician with greater tactile sensitivity. Hygienists using dull curettes subgingivally will feel much less, as the rounded cutting edge slides over calculus deposits. A sharp cutting edge will catch on the deposit, and the clinician will feel it more readily.
“Sharp cutting edges remove calculus deposits cleanly. A great hygienist with excellent technique working subgingivally with a dull blade can remove some or even most of a deposit, but will invariably leave some calculus burnished to the tooth.
“For hygienists to deliver the highest quality care, they need to have sharp instruments to do their job effectively.”
Risks to clinicians
Dull instruments also pose dangers to the short- and long-term health of clinicians. Anne Guignon, MPH, RDH, CSP, one of the industry’s biggest advocates for ergonomic health, said that “Dull instruments are horrible and require a tighter pinch grip, which creates fatigue and reduces tactile sensitivity, and increases the force and pressure a clinician has to use to try to remove deposits. Dull instruments decrease the likelihood for thorough deposit removal. Increased force, pressure, and a tight pinch grip strains the muscles, ligaments, and tendons in the fingers, hands, wrist, forearm, elbow, upper arm, shoulder, and upper back. Dull instruments waste valuable clinical time and increase patient discomfort.”
Conclusion
In the results of our survey, we were surprised to see that the amount of instrument sets a hygienist had access to didn’t dramatically influence how often the instruments were sharpened. For example, about the same percentage of hygienists sharpened their instruments once a week, regardless of whether they had four sets or twelve. It even seems as if our respondents who had access to only four were actually more likely to sharpen only once every one to three months, versus those who had access to more (table 1).
Dull instruments are a risk—not only to patients, but also to hygienists themselves and even to the financial sustainability of a practice. It bears mentioning that Wanless’s article mentioned earlier also discusses the ethical consequences of leaving calculus behind, namely supervised neglect. “A diligent clinician would never deliberately leave calculus, let alone burnished calculus. But what if you learned today that you were leaving deposits, contributing to chronic gingival disease? Are you unintentionally practicing supervised neglect?” she asks.4
The daily practice of hygiene can prove more complicated. Hygienists have many pressures that get in the way of sharpening, so if sharpening regularly at the practice is just not feasible, it’s important to note that there are other options, such as sharpening services (Nordent Manufacturing, among others) or automated machines. For a helpful discussion of your options, see Patricia Pine’s June 2018 article in RDH, “DIY, or get the service?”
References
1. Geisey N. Digging past positioning: Hydration, sleep, and sharp instruments influence ergonomic health too. https://www.rdhmag.com/articles/print/volume-37/issue-4/contents/digging-past-positioning.html. RDH website. Published April 1, 2017. Accessed November 6, 2018.
2. DeStefano AW. The ballad of time, money, and instrument sharpening. https://www.rdhmag.com/articles/print/volume-38/issue-9/content/the-ballad-of-time-money-and-instrument-sharpening.html. RDH website. Published September 1, 2018. Accessed November 6, 2018.
3. Watterson DG. No more dull instruments! https://www.rdhmag.com/articles/print/volume-32/issue-5/features/no-more-dull-instruments.html. RDH website. Published May 1, 2012. Accessed November 6, 2018.
4. Wanless T. The role of hygienists in recognizing and healing supervised neglect related to burnished calculus. https://www.rdhmag.com/articles/print/volume-37/issue-6/contents/supervised-neglect.html. RDH website. Published June 1, 2017. Accessed November 6, 2018.