Abstract: Numerous studies show the link between cancer and inflammation and their involvement with periodontal disease. The impact of cancer treatment proves to significantly affect one’s health. The aim of this literature review is to determine whether cancer treatment will negatively affect the periodontal condition and oral health.
In total, 28 reviews—including cohort, cross-sectional, case-control, and systematic reviews—dated within the past 10 years were carefully examined. The study population consists of individuals with both periodontal disease and cancer diagnoses. This review examines the effects of cancer treatments on the periodontium and the recommended preventive dental hygiene strategies as directed by a dental clinician.
Recent studies show a correlation between inflammation-induced pathogens and cancer growth. They also show that there was a significant increase of periodontal pathogens—such as Porphyromonas gingivalis, Treponema denticola, Tannerella forsythia, and Aggregatibacter actinomycetemcomitans—found in the oral cavity of patients with periodontal disease. These bacteria contribute to the destruction of the periodontium and normal cells, while forming carcinogenic cells in the process. Likewise, certain cancer treatments destroy healthy cells in the oral cavity.
Pediatric cancer care and the dental professional
Inflammation: A major link between oral and systemic diseases
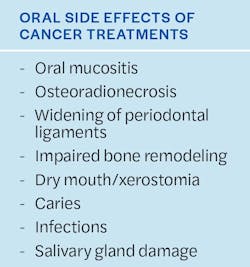
Cancer treatments have undesirable side effects, including oral mucositis, osteoradionecrosis, and xerostomia. These side effects increase the number of pathogens in the mouth and impair bone remodeling. Numerous studies have shown that performing periodontal treatment to remove harmful pathogens significantly reduces the risks associated with cancer formation.
Most patients were reported to be in generally poor oral health prior to cancer treatment. Dental clinicians should stress the importance of prevention and completion of dental treatment to improve patients’ quality of life. From this data, we can conclude that the effects of cancer treatment negatively affect the periodontal condition and overall oral health.
Introduction
Many adults live day-to-day with undiagnosed and untreated periodontal disease (PD). Meyer et al. reported that PD is a chronic infection caused by bacteria that creates inflammation of the gingiva and leads to destruction of the tissues and bone supporting the teeth.1 It is no secret that PD can contribute to the progression of many other systemic diseases.
Specifically, cancer has remained one of the leading causes of death in the world. According to a study completed by Torre in 2012, nearly 300,400 new cancer cases were diagnosed, and an estimated 145,400 deaths occurred from head and neck cancer.2 A wide variety of cancer treatments are available but the most common include surgery, chemotherapy, radiation, and a combination of surgery and radiation or chemotherapy.3 These cancer treatments have undesirable side effects and an overall negative effect on a person’s body and health, including oral hygiene.4 Studies show that there is a connection between PD and an increased risk of cancer.5
Inflammation is the constant link in the relationship between PD and cancer.5 The immune system’s response to these inflammatory indicators is thought to be the main correlation between the two.5 Cancer treatments affect different regions of the body. For example, the effects of surgery and radiation therapy are limited to specific parts of the body, while chemotherapy inhibits all cell growth and living cells.4 This means that malignant or toxic cells and healthy cells are all affected concurrently during treatment. Cancer treatments have many other negative effects on the oral cavity, including dental caries, xerostomia, and mucositis.3
Studies have shown that periodontal treatment can lower inflammatory indicators and reduce risks associated with cancer within two to six months of treatment completion.5,6 But studies have also shown that noncompliance is a major issue with patients.3,7 One study stated that 97% of patients needed dental treatment before beginning cancer treatment, but only 81% completed the recommended restorative dental work.7 Stressing the importance of practicing good oral hygiene habits routinely, early detection, and effective treatment are necessary to ensure a better quality of life.4,8 The objective of this literature review is to evaluate the effects of cancer treatment on periodontal health. The research question of this literature review is: For patients undergoing cancer treatment, will cancer treatments worsen PD and overall oral health?
Inflammation and cancer
PD is an irreversible disease that affects the supporting structures and tissues of the oral cavity.1,4,9-13 Common characteristics associated with PD include increased bleeding, worsening of periodontal pocket depths, bone loss, tooth mobility, gingival recession, and inflammation.9-12 Together they destroy the gingiva, ligaments, and bone that make up the oral cavity.1,4,6,9-12 Ultimately, if left untreated, PD leads to tooth loss.10-12
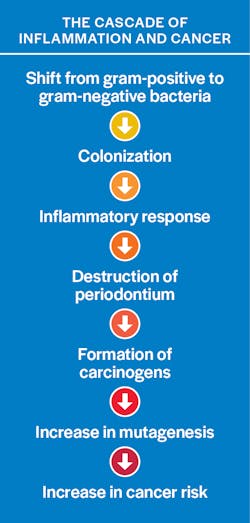
The formation of periodontal pathogens begins with a shift from gram-positive bacteria to gram-negative organisms.1 The most commonly found pathogens in a patient with PD include P. gingivalis, T. denticola, T. forsythia, and A. actinomycetemcomitans.1,11-14 Although many of these harmful organisms can be found in the mouth of a healthy person, they are typically recorded at lower levels, causing little to no damage.1 As the bacteria begins to colonize and become more aggressive, they initiate an inflammatory response that triggers the destruction and breakdown of the periodontum.1,11 The immune system’s response to inflammation plays a major role in the correlation to cancer formation.1,5
Meyer et al. explains that the connection between cancer and inflammation has been acknowledged in countless publications dating back to more than a century ago.1 These studies have shown that the inflammatory markers resulting from PD are the main link to cancer.1,5,6,9-10 From this, we have learned that the chronic inflammation produced by harmful periodontal organisms is what initiates the destruction of normal cells and formation of carcinogens.1 Further, Sun et al. state, “chronic exposure to inflammatory mediators, including neutrophils, monocytes, macrophages, or cytokine metabolites, has been suggested to increase cell proliferation and mutagenesis, thereby leading to cancer.”14 With regard to the current information, it is clear that the development of cancer suppresses the immune system’s response and sets off a chain reaction that aids in the formation of increased harmful pathogens throughout the body.5
Effects of cancer treatments
The type of cancer treatments administered varies from person to person depending on the size and location of the lesions.4 Chemotherapy uses drugs to kill cancer cells and can be administered to a patient in many ways, including oral or intravenous delivery.4 Radiation therapy uses radiation in high or low doses to target and damage the actual DNA of cancer cells.15,16 The dosage is subjective to cancer location, size, and how aggressive the treating physician is trying to be with respect to the patient’s wants or needs.4 Surgery simply aids in removing the cancer site from the body. Together these treatments help kill, shrink, slow the growth, and prevent the reproduction of cancer cells, but they can also help ease the symptoms cancer patients are subjected to.16 Some therapies not only aid in destroying cancer cells, but they destroy healthy cells in the process as well.4,16
One study verified that prior to the start of cancer treatment, 95% of patients were already diagnosed with PD.15 In this regard, cancer therapies have many negative effects on the body and can advance the progression of PD.4,15,16 In a study conducted by Vera Llonch et al., it was confirmed that oral mucositis occurred in 83% of patients as a side effect of chemotherapy or radiation treatment.17 Oral mucositis refers to painful mouth sores caused by the formation of ulcerative lesions as a direct result of cancer treatment.17 This not only causes extreme discomfort for patients; it also creates a doorway for the entry of periodontal pathogens.17 Patients with head and neck cancer treated with radiation therapy often develop osteoradionecrosis of the jaw.7,15 Osteoradionecrosis results in the destruction of bone and bone-repairing abilities, is very hard to treat, and often leads to loss of clinical attachment of the gingiva and tooth loss.7,15
Similarly, cancer treatment affects the blood vessels surrounding the teeth, which leads to widening of the periodontal ligaments and an increased chance of impaired bone remodeling.16 Radioactive iodine is another type of cancer treatment, specifically for thyroid cancer, that uses an oral iodine to emit radiation and destroy cancer cells.18 One study reported 44% of patients experienced dry mouth after radioiodine treatment, which luckily is easily treatable.18
There are many other side effects from cancer treatments to the oral cavity, including xerostomia, dental caries, and infections.3,19,20 Damage to salivary glands is a common symptom from radiation treatment. Lack of salivary flow disturbs pH buffering of the mouth and increases the chance of dental caries and infection causing bacteria to form.3,21 We know that dry mouth can lead to dental caries, but we forget that it can lead to swallowing and eating problems too.21 As a result, many cancer patients have food remaining in the oral cavity for hours, which increases the formation of dental caries.2 Many of these symptoms from cancer treatment contribute to noncompliance in patients with regard to necessary home care and periodontal treatment.7
Preventive strategies
Receiving the proper dental diagnosis and treatment prior to cancer treatment can help reduce the progression of PD and one’s risk of cancer.14,22 Many studies stated that patients typically reported to dental offices while already in poor oral health and that a cancer diagnosis did not change an individual’s hygiene habits.3,7 Simply put, stressing the importance of improving the quality of life is necessary for change.4,8 Reducing inflammation-causing pathogens in the oral cavity will slow the development and progression of tumors.23 This can be done by scaling subgingivally on patients with periodontitis every three to four months or when allowed by the treating physician.14 Application of a fluoride varnish at each visit can also decrease caries formation.3
Prevention is key when it comes to treating patients. It is the duty of dental clinicians to provide patients with the necessary tools to practice good oral hygiene daily.8 One study confirmed that poor oral hygiene specifically increases an individual’s risk of cancer.24,25 It is extremely important for clinicians to give patients detailed oral hygiene instructions about brushing after meals, flossing daily, using prescription mouthrinse as directed, and completing any necessary dental treatment. Cancer patients deal with many complications from treatments. Advising them on how to care for the mouth during this time is extremely beneficial.4 Recommending saliva substitutes (lozenges, sprays, gels) to patients with xerostomia can help with saliva production and soothe the mouth.3,19 Remind periodontal patients who are undergoing cancer treatment to avoid alcohol-containing mouthrinses and whitening toothpastes, because they will irritate the mouth.19,25 Advise patients that while eating, avoid sugar and spicy or acidic foods or beverages, and to stay well hydrated with water.19
Conclusion
Cancer has remained one of the leading causes of death worldwide for quite some time. Depending on the stage and location of the cancer, most forms are treatable. However, there are many downsides to cancer treatment, which include the risk of treatment not working, undesirable side effects, and the chance the cancer may return over time. Cancer treatment also presents an individual with the high probability of negatively affecting the periodontal condition. Recent studies confirm that there is a direct correlation between cancer and the inflammation that causes PD.
Currently, it is understood that the formation of pathogens can lead to PD. In turn, these pathogens can aid in the formation and growth of different types of cancer. When a patient with PD is being treated for cancer, the oral cavity is constantly being subjected to many changes, including the formation of harmful pathogens, the destruction of healthy cells, and an endless list of harmful side effects. Some of these are short-term, while others can cause long-term damage along with many complications. It is the dental clinician’s duty to provide patients with recommendations on how to care for the mouth during this challenging time.
The studies mentioned in this article draw the conclusion that cancer treatment does in fact worsen a patient’s PD and overall oral health. Stressing with patients early on the importance of completing any necessary dental treatment before cancer treatment is a major role the clinician needs to play. A thorough explanation on how the mouth will be affected by cancer treatment and how to care for it will offer more comfort to the patient. Educating your patients about the importance of practicing good oral hygiene habits daily and getting routine dental cleanings will help ensure they have a better quality of life.
Editor's note: This article appeared in the November 2022 print edition of RDH magazine. Dental hygienists in North America are eligible for a complimentary print subscription. Sign up here.
References
- Meyer MS, Joshipura K, Giovannucci E, Michaud DS. A review of the relationship between tooth loss, periodontal disease, and cancer. Cancer Causes Control. 2008;19(9):895-907. doi:10.1007/s10552-008-9163-4
- Bressan V, Stevanin S, Bianchi M, Aleo G, Bagnasco A, Sasso L. The effects of swallowing disorders, dysgeusia, oral mucositis and xerostomia on nutritional status, oral intake and weight loss in head and neck cancer patients: a systematic review. Cancer Treat Rev. 2016;45:105-119. doi:10.1016/j.ctrv.2016.03.006
- Jham BC, Reis PM, Miranda EL, et al. Oral health status of 207 head and neck cancer patients before, during and after radiotherapy. Clin Oral Investig. 2008;12(1):19-24. doi:10.1007/s00784-007-0149-5
- Vozza I, Caldarazzo V, Polimeni A, Ottolenghi L. Periodontal disease and cancer patients undergoing chemotherapy. Int Dent J. 2015;65(1):45-48. doi:10.1111/idj.12133
- Hwang IM, Sun LM, Lin CL, Lee CF, Kao CH. Periodontal disease with treatment reduces subsequent cancer risks. QJM. 2014;107(10):805-812. doi:10.1093/qjmed/hcu078
- Michaud DS, Liu Y, Meyer M, Giovannucci E, Joshipura K. Periodontal disease, tooth loss, and cancer risk in male health professionals: a prospective cohort study. Lancet Oncol. 2008;9(6):550-558. doi:10.1016/S1470-2045(08)70106-2
- Niewald M, Fleckenstein J, Mang K, Holtmann H, Spitzer WJ, Rube C. Dental status, dental rehabilitation procedures, demographic and oncological data as potential risk factors for infected osteoradionecrosis of the lower jaw after radiotherapy for oral neoplasms: a retrospective evaluation. Radiat Oncol. 2013;8(227):1-12. doi:10.1186/1748-717X-8-227
- Yan R, Chen X, Gong X, Wang J, Yu J. The association of tooth loss, toothbrushing, and quality of life among cancer survivors. Cancer Med. 2018;7(12):6374-6384. doi:10.1002/cam4.1835
- Tezal M, Sullivan MA, Hyland A, et al. Chronic periodontitis and the incidence of head and neck squamous cell carcinoma. Cancer Epidemiol Biomarkers Rev. 2009;18(9):2406-2412. doi:10.1158/1055-9965.EPI-09-0334
- Javed F, Warnakulasuriya S. Is there a relationship between periodontal disease and oral cancer? A systematic review of currently available evidence. Crit Rev Oncol Hematol. 2016;97:197-205. doi:10.1016/j.critrevonc.2015.08.018
- Lobáo WJM, Carvalho RCCDE, Leite SAM, et al. Relationship between periodontal outcomes and serum biomarkers changes after non-surgical periodontal therapy. An Acad Bras Cienc. 2019;91(2):1-10. doi:10.1590/0001-3765201920170652
- Wen BW, Tsai CS, Lin CL, et al. Cancer risk among gingivitis and periodontitis patients: a nationwide cohort study. QJM. 2014;107(4):283-290. doi:10.1093/qjmed/hct248
- Vargas-Villafuerte KR, Dantas FT, Messora MR, et al. Preliminary results of non-surgical periodontal treatment in patients with breast cancer undergoing chemotherapy. J Periodontol. 2016;87(11):1268-1277. doi:10.1902/jop.2016.160101
- Sun J, Zhou M, Salazar CR, et al. Chronic periodontal disease, periodontal pathogen colonization, and increased risk of precancerous gastric lesions. J Periodontol. 2017;88(11):1124-1134. doi:10.1902/jop.2017.160829
- Schuurhuis JM, Stokman MA, Witjes MJH, et al. Patients with advanced periodontal disease before intensity-modulated radiation therapy are prone to develop bone healing problems: a 2-year prospective follow-up study. Support Care Cancer. 2018;26(4):1133-1142. doi:10.1007/s00520-017-3934-y
- Ammajan RR, Joseph R, Rajeev R, Choudhary K, Vidhyadharan K. Assessment of periodontal changes in patients undergoing radiotherapy for head and neck malignancy: a hospital-based study. J Can Res Ther. 2013;9(4):630-637. doi:10.4103/0973-1482.126461
- Vera-Llonch M, Oster G, Hagiwara M, Sonis S. Oral mucositis in patients undergoing radiation treatment for head and neck carcinoma. Cancer. 2006;106(2):329-336. doi:10.1002/cncr.21622
- Walter MA, Turtschi CP, Schindler C, Minnig P, Muller-Brand J, Muller B. The dental safety profile of high-dose radioiodine therapy for thyroid cancer: long-term results of a longitudinal cohort study. J Nucl Med. 2007;48(10):1620-1625. doi:10.2967/jnumed.107.042192
- Pinna R, Campus G, Cumbo E, Mura I, Milia E. Xerostomia induced by radiotherapy: an overview of the physiopathology, clinical evidence, and management of the oral damage. Ther Clin Risk Manag. 2015;11:171-188. doi:10.2147/TCRM.S70652
- Hong CHL, Napeñas JJ, Hodgson BD, et al. A systematic review of dental disease in patients undergoing cancer therapy. Support Care Cancer. 2010;18(8):1007-1021. doi:10.1007/s00520-010-0873-2
- Fitzpatrick SG, Katz J. The association between periodontal disease and cancer: a review of the literature. J Dent. 2010;38(2):83-95. doi:10.1016/j.jdent.2009.10.007
- Shin YJ, Choung HW, Lee JH, Rhyu IC, Kim HD. Association of periodontitis with oral cancer: a case-control study. J Dent Res. 2109;98(5):526-533. doi:10.1177/0022034519827565
- Salazar CR, Francois F, Li Y, et al. Association between oral health and gastric precancerous lesions. Carcinogenesis. 2011;33(2):399-403. doi:10.1093/carcin/bgr284
- Shakeri R, Malekzadeh R, Etemadi A, et al. Association of tooth loss and oral hygiene with risk of gastric adenocarcinoma. Cancer Prev Res (Phila). 2013;6(5):477-482. doi:10.1158/1940-6207.CAPR-12-0491
- Guha N, Boffetta P, Wünsch Filho V, et al. Oral health and risk of squamous cell carcinoma of the head and neck and esophagus: results of two multicentric case-control studies. Am J Epidemiol. 2007;166(10):1159-1173. doi:10.1093/aje/kwm193