HPV and oral sex: You want me to discuss what with my dental patients?!
You want me to discuss what with my patients?!
By Catrice Opichka, RDH
Do you remember when smoking cessation discussions were the most difficult conversations we had with our patients? Do you recall the first battles we had discussing the harmful effects of chewing tobacco? The discussion of smoking and chewing as risk factors for oral cancer have become, for many of us, as common as discussing the effects of bacteria in periodontal disease. In the 21st century, smoking and chewing are among the easier topics we have to discuss with our patients. The human papillomavirus (HPV) has changed the way we look at cancer risk and detection, making patient education a bit more complicated.
Twenty years ago, if someone had told me that I would be finding ways to educate patients about the risks of early sexual behavior on their oral health, I would have said, "Not a chance." However, that is exactly what has happened.
The facts about HPV and oral cancer
HPV is the most common sexually transmitted infection in the United States. Although most types of HPV are not harmful to people, more than 40 strains can infect the genital areas, as well as the mouth and throat, and these can cause cancer. Because HPV is often asymptomatic, most people who become infected do not know they have the virus. For the majority of individuals, the infection clears up on its own. For some people, however, the virus interferes with the normal cell function that prevents excess growth, leading to precancerous cells and eventually cancer.1
Recent reports are showing that, in medical centers across the United States, HPV is now responsible for more than half of all oropharyngeal cancers diagnosed.2 According to the Oral Cancer Foundation, HPV is now the leading cause of all oropharyngeal cancers.3 However, most dental professionals rarely discuss this disease with their patients. Discussing the cause-and-effect relationship between oral sex and oral cancer is not easy for anyone, but since 80% of individuals in the United States will become infected with HPV in their lifetimes, it is a topic worth investigating and sharing with our patients.3
Changing trends in sexual behaviors
There are several reasons that HPV-related cancers are on the rise. One of the most significant factors is the changing sexual behavior of our adolescent patients.
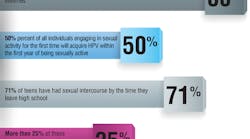
Fifty percent of all individuals engaging in sexual activity for the first time will acquire HPV within the first year of being sexually active, and the risk of HPV increases with every sexual partner. It is estimated that 71% of teens have had sexual intercourse by the time they leave high school, and more than 25% of these teens have had more than one sexual partner.4
Another factor is the mindset that many teenagers currently have toward oral sex. If we were to ask a group of teenagers if oral sex counts as sexual behavior, the majority would say that it does not. Eighty percent of sexually active people, ages 14 to 44, have had oral sex with a partner of the opposite sex.5
Would increasing education about the effects of sexual behaviors make a difference in this trend? A study published in the Journal of Sex Research tested the effects of oral sex and HPV-risk education on young adults' sexual behaviors.4 The research concluded that there were several positive effects of the education provided, including reported changes in oral sex behaviors and an increase in preventive measures taken, such as a greater likelihood of considering the HPV vaccination.4
As dental professionals, we can do many things to help fight HPV-related oral cancer. Of these, I believe we should focus on the following two in clinical practice.
The oral cancer exam
If you ask a room full of dentists and dental hygienists if they do oral cancer screenings on every patient at every visit, the answer is most often "no." Two-thirds of all dental hygienists admit to doing intraoral examinations only when the patient is known to be a heavy smoker or user of chewing tobacco. However, many patients diagnosed with oropharyngeal cancer have never smoked or used chewing tobacco. If we continue to limit our cancer screenings to patients with "traditional risk factors," oral cancers will go undiagnosed.
We also need to consider the locations where HPV-related oral cancer is typically found and how those differ from areas where tobacco users might be more prone to develop cancer. The most common locations for HPV-related oral cancer are: in the posterior of the mouth, on the tonsils, on the tonsillar pillar, at the base of the tongue, and on the oropharynx. Along with providing a thorough intraoral and extraoral inspection, it is also critical that we incorporate appropriate patient interview questions in order to investigate potential changes that may be signs of early oropharyngeal cancer.
Feeling rusty? Continuing education is essential for brushing up on your skills when you haven't used them in a while. Whether you take a refresher course in oral pathology or attend a seminar on oral cancer screening and new detection technology, it is important to feel comfortable with your cancer detection skills. The Oral Cancer Foundation, American Cancer Society, and other organizations provide valuable online resources that we can review to improve our abilities to diagnose oral cancer.
The oral cancer exam can also be a fantastic tool to open the door for patient education. Verbally walking patients through the exam makes them aware of the high level of care you are providing, and it allows you to teach as you examine.
HPV education
Discussing HPV is not easy, and there are a number of things to take into consideration before embarking on a new mission to spread the word about this issue and the behaviors that put our patients at risk. I am not suggesting that we all go into our offices tomorrow and start talking about oral cancer and oral sex. The journey to becoming comfortable with educating our patients about HPV is a little like climbing a mountain. Having a plan is the first step in creating a protocol for the whole office.
1. Start at basecamp-The first step in creating a protocol for HPV education takes place within the dental team. Like implementing any system in the dental practice, everyone needs to be on board and have an understanding of what is expected in communication with patients. The whole team needs to understand the importance of the cancer exam and the education that follows. It is imperative to have everyone "speaking the same language" when discussing HPV to ensure that we do our best to use terminology that will not be offensive to patients.
The best way to ensure that everyone understands their roles in HPV education is to set time aside for educating the entire team. Remember, even among the dental team, there will be individuals who are more comfortable with this topic than others. The agenda for these team meetings may differ from practice to practice, but common exercises should include creating a written and verbal protocol, roleplaying, and pursuing continuing education about pathology, cancer detection, and patient communication.
2. Create the map-Creating written and verbal protocols for the practice will help to map out procedures and guidelines for discussing HPV. Creating a consent form for discussing HPV with minors and incorporating new medical history questions are just a couple of ways that we can introduce HPV education into our practices. The Oral Cancer Foundation and Centers for Disease Control are excellent resources for educational materials, such as pamphlets and brochures, to offer patients.
3. Prepare-Continuing education is the key to achieving successful results. Nevertheless, many of us barely feel comfortable talking about HPV, much less facilitating a team meeting to train the rest of the individuals in our offices. Fortunately, there are resources and organizations that can help. Consider asking an oral surgeon in your community to come into your practice to discuss pathology. You can invite a representative from a company that manufactures cancer-screening technology, such as OralID or LED Dental, to demonstrate the latest tools in cancer detection devices. Dental study groups, such as the Seattle Study Club, provide advanced education on the most relevant topics in dentistry, and they incorporate these topics into their yearly curriculum. These resources can help provide the necessary training to prepare your team.
4. Train, train, train-You wouldn't attempt to climb to the summit of Mt. Everest after lacing up your hiking boots for the first time. Starting small and practicing is essential to achieving big goals. Everything we do that seems uncomfortable in the beginning eventually becomes fluid after practice. (OK, maybe climbing Everest isn't fluid for anyone, but you get the point!) Conversations about HPV, the risk of oral cancer, and the sexual behaviors that increase that risk will all become easier with practice.
HPV can be difficult to discuss. However, getting the dental team on board with improved cancer detection, a protocol for patient education, and the tools necessary for excellent communication will allow us to conquer the challenge of HPV education for our patients. RDH
Catrice Opichka, RDH, has been active in the field of dentistry for 26 years and has practiced as a registered dental hygienist for the last 18 years. She owns Pure Education LLC, lectures internationally, teaches clinical dental hygiene at PIMA Medical Institute, and is a member of the Seattle Study Club Education Advisory Board. Catrice lectures on treating the oncology patient, HPV and oral cancer risk, the oral effects of addiction, and complex communication in the clinical setting. To learn more about this topic, contact Catrice at [email protected] or (920) 246-4165.
References
1. HPV and Cancer. National Cancer Institute. http://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-fact-sheet.
2. HPV-Associated Cancers Statistics. Centers for Disease Control and Prevention. http://www.cdc.gov/cancer/hpv/statistics/. Updated September 2, 2014.
3. The HPV Connection. Oral Cancer Foundation. http://oralcancerfoundation.org/hpv/. Updated April 2014.
4. Stock ML, Peterson LM, Houlihan AE, Walsh LA. Influence of oral sex and oral cancer information on young adults' oral sexual-risk cognitions and likelihood of HPV vaccination. J Sex Res. 2013;50(1):95-102.
5. Copen CE, Chandra A, Martinez G. Prevalence and timing of oral sex with opposite-sex partners among females and males aged 15-24 years: United States, 2007-2010. National Health Statistics Reports. 2012;56:1-14. http://www.cdc.gov/nchs/data/nhsr/nhsr056.pdf. Published August 16, 2012.