A link between Alzheimer’s disease and oral inflammation: The dental hygienist’s role
The general population may not understand that inflammation anywhere in the body must be mediated throughout the whole organism to be effective at the site of inflammation itself. When a person gets a headache, he or she might take a pill that results in relief. However, the person may not even think about how the swallowing of a pain pill for any kind of pain results in relief of the headache!
Our patients learn this from us through repeated maintenance visits if they are lucky. Lucky, because as dental hygienists we tend to focus on keeping the mouth clean, as expected, but possibly neglect the links to systemic health.
Becoming specialized in our thinking mirrors the thinking of the patient. General practice physicians refer specific issues to specialists, so, the patient thinks of us as “mouth specialists.” By digging into our wide educational background, we need to expand the conversation to inform the patient of the oral-systemic link.
After an examination by the dentist, patients are usually “booked” in with the dental hygienist. As dental professionals, we know why, but the amount of time during a workday precludes explaining the reason to the patient. Patients have become used to this routine of care that they do not question the reasons behind it. Not being mind readers, one can surmise the patient thinks that their teeth are “dirty” and need to be cleaned before dental treatment on the teeth themselves can be undertaken by the dentist.
In following this routine, we are relegating ourselves to the role of “the cleaning person.” Dental hygienists are much more. The amount of knowledge a student must gain before being granted access to a license is mind-boggling. Much of the learning must be compressed to fit in with university timelines, so dental professionals are expected to take continuing education courses throughout their professional careers. This expectation is the basis for ongoing licensing to practice. As dental hygienists are humans first, the easier way is sought. Courses that need deeper biological learning may be foregone in favor of the easier course on the procedures of tooth whitening.
To encourage our patients to value their oral health, the dental hygienist must delve into biological reasons for health and disease and the homeostasis the body craves. Diabetes, cardiovascular disease, cancer, low birth-weight and pre-term babies, obesity, gastrointestinal problems, and now Alzheimer’s disease are showing connections to oral inflammation. The observant reader will say that there are genetics involved here! Of course! However, the mitigation of inflammation will slow the progression of the disease.
Alzheimer’s disease (AD) is devastating to patients and their families. The disease begins earlier than many people suspect. It may be a slow loss of memory, but to have such a symptom, the person needed to have deterioration that began years or decades ago. Dental hygienists are aware of many diseases and can connect them to inflammation elsewhere. The patient really does not know this. It is up to us to educate them on the links.
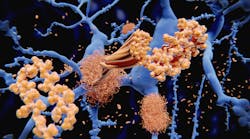
Many theories circulate on the etiopathogenesis of AD. One is the amyloid hypothesis, another is the inflammation theory, and yet another brings to light specific bacterial invasion of the brain tissues. When AD brain tissue is studied microscopically in autopsies, there appears to be patches of specific proteins. The two most recognized proteins involved in the disease are amyloid beta (Aβ) and tau tangles. Aβ is an antibacterial, antifungal, and antiviral innate immune initiator produced due to the presence of microorganisms.1 This protein, Aβ, is generated in the brain and surrounding tissues and acts as a tie to other receptors. Aβ can be transported between tissues and even across the blood-brain barrier through many complex pathways, where it initiates proinflammatory activities in response to microorganism activity.2,3
Scientific data suggests inflammation as a connection between the mouth, mind, and body. The medical consequences of forgetting those connections result in severe disturbances of homeostasis. Within dental practices, the dental professional specializes on the mouth by optimizing patient compliance for dental health. But in medical offices, doctors focus on the optimizing total wellness and the patient’s quality of life rather than regular dental appointments. While separation in services by health-care professionals exists, the challenge of inflammation may not be considered. Dental hygienists need to be cognizant of the many contributors of inflammation in the human body. Contributors include genetics, sleep apnea, rheumatoid arthritis, insulin resistance, and second-hand smoke in addition to the person’s genetic proclivity for periodontitis.
With an arrest of oral inflammation, there should be a reduction of inflammation throughout the body via the circulatory system. Oral health can be achieved through meticulous care taken during brushing and flossing. The lack of bleeding on these activities does not demonstrate a lack of inflammation in the mouth (for example, as with smokers). Patients should be advised to have a full periodontal check-up. Dementia and AD gives no advance warning much like oral disease with no warning symptoms.
This information serves as an incentive to explore the relationship between inflammation and periodontal disease in further detail. One simple connection is the presence of inflammation in any location in the body. Human immune systems can handle only so much. Adding to the chronic nature of regular inflammation, oral disease can lead to the inability of coping with normal life stresses.
References
1. Fülöp T, Itzhaki RF, Balin BJ, Miklossy J, Barron AE. Role of microbes in the development of Alzheimer's disease: State of the Art - An International Symposium Presented at the 2017 IAGG Congress in San Francisco. Front Genet. 2018;9:362. doi: 10.3389/fgene.2018.00362
2. Paris D, Town T, Parker TA, et al. Inhibition of Alzheimer's beta-amyloid induced vasoactivity and proinflammatory response in microglia by a cGMP-dependent mechanism. Exp Neurol. 1999;157(1):211-21. doi: 10.1006/exnr.1999.7055
3. Tanzi RE, Moir RD, Wagner SL. Clearance of Alzheimer's Abeta peptide: the many roads to perdition. Neuron. 2004;43(5):605-8. doi: 10.1016/j.neuron.2004.08.024
Sabrina Heglund, PhD, MHS, BDSc, Dip(DH), is a Canadian dental hygienist who travelled to Karachi, Pakistan and remained there for 2.5 years in 2018. Sabrina refined the curriculum and clinical practice for the associate of science in dental hygiene degree at the Aga Khan University. Her doctoral thesis featured the role of neutrophils in the gingival crevicular fluid of healthy and periodontally compromised patients. Sabrina has volunteered on many fronts to assist indigenous people, disadvantaged homeless folks, and professional organizations to further educate populations on dental health and its connections to systemic health.