by Lynne Slim, RDH, BSDH, MSDH
During the early 19th century, it was discovered that adding yellow (now called white) phosphorous to matchstick heads made it easier to ignite matches. As a result, there was an enormous demand for these “strike-anywhere” matches.1 During the industrial revolution, this new industry of matchmaking was profitable, and low wage workers spent 10 to 15 hours a day over large heated vats that contained yellow phosphorus.2
The phosphorous vapors were breathed in by workers and combined with other chemicals in the body to produce a potent nitrogen-containing bisphosphonate. Today’s oral nitrogen-containing bisphosphonates and intravenous nitrogen-containing bisphosphonates circulate around the body the same way as the phosphorous vapors, and are absorbed into bone and ingested by osteoclasts. When this unique binding process of bisphosphonates to bone occurs, osteoclasts are poisoned, and this reduces or eliminates bone turnover. Alveolar bone in the mandible and maxilla turns over more rapidly than in long bones, so the jaws are a better target for bisphosphonate toxicity.2
The first case of “phossy jaw” was recorded in 1838, and the victim, a female Viennese matchstick maker, had been exposed to the phosphorous vapors over a five-year period. Back then, the average time between exposure to the phosphorous vapors and the appearance of “phossy jaw” was about five years, but only about 5% of those exposed were inflicted with this disfiguring and often lethal affliction.1
Poor factory working conditions, especially in England, fostered the disease, and even Queen Victoria’s advisors investigated phossy jaw. But it wasn’t until the early 1900s that the production of phosphorous matches was outlawed in the United Kingdom. Other countries such as Finland, Denmark, Sweden, and Switzerland quit using yellow phosphorous sooner, and the United States placed heavy taxes on phosphorous matches.1
To better grasp the extensive debilitation of phossy jaw, here is a case description from the Odontologic Museum, Royal College of Surgeons, in London, England.
“The patient was a 35-year-old matchmaker who presented with great external swelling and in a debilitated state from inability to take solid food. Extending from ear to ear along the line of the jaw was a chain of ulcerated openings, from which there was profuse discharge and through any of which a probe could reach dead bone. Inside the mouth, the toothless alveolar process was seen bared of soft parts in its whole extent, the bone being rough and brownish-black. The gum gaped widely away from the dead jaw and had receded so as to leave it above the natural level of that bone, a probe could be passed easily either in front or behind the bone toward the sinuses of the neck. Under chloroform, the jaw was removed by dividing it at the symphysis and dragging the two halves out separately.”2
Epidemiology of BIONJ
It wasn’t until 2003 that today’s intravenous and oral nitrogen-containing bisphosphonate medications were implicated as major risk factors in the development of exposed necrotic bone of the jaws.2 Since then, a literature review of case reports from around the world has been published and a summary of epidemiological data surrounding these cases has been reported. (See Table 1)3
Most of the researchers who reported cases of bisphosphonate-induced osteonecrosis of the jaw (BIONJ) found that these patients were treated with zoledronate, pamidronate, or a combination of these drugs, which are commonly used for treating breast cancer or myeloma. In about 5% of cases, subjects with BIONJ were being treated for osteoporosis. Precipitating events that contribute to BIONJ are tooth extractions (about 50% of cases), mandibular exostoses, periodontal disease, and local trauma from ill-fitting dentures. It is not known if the placement of dental implants is a precipitating factor, and a recent study implicates smoking and obesity as possible risk factors. It is also common for BIONJ subjects to be taking cytotoxic drugs and glucocorticoids.3
Intravenous nitrogen-containing bisphosphonates are commonly prescribed for managing skeletal complications of malignancy, including metastatic bone disease (cancer that metastasizes to bone) and hypercalcemia of malignancy (abnormal amount of calcium in the blood).4 When given intravenously, it takes only a year for nitrogen-containing bisphosphonates to saturate bone, and many researchers have reported the risk of intravenous BIONJ to be 5% to 15%.5
Osteoporosis and oral nitrogen- containing bisphosphonates
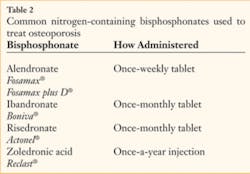
BIONJ is also associated with the oral administration of nitrogen-containing bisphosphonates to treat osteoporosis. (See Table 2 for some common names of oral bisphosphonates.)6 To date, epidemiological evidence linking BIONJ to oncology patients treated with intravenous bisphosphonates is stronger and more reliable than data surrounding oral bisphosphonate use.3 In the risedronate (Actonel®) and alendronate (Fosamax®) clinical trials of 16,000 to 17,000 patients, no cases of BIONJ were reported, but post-marketing surveys conducted to mid-2007 indicated an incidence of <1.2 per 100,000 patient-years for risedronate and <0.5 to 2.5 per 100,000 patient-years for alendronate. To date, the prevalence of BIONJ associated with oral bisphosphonates is approximately one per 100,000 patient-years, and it has been reported that this is not too different from that reported in the general population.3 The number of patients taking bisphosphonates for osteoporosis and other metabolic bone diseases such as Paget’s disease is much greater than patients with cancer. Therefore, even a low incidence of oral-induced BIONJ may be significant.7
A couple of studies reported higher risk of BIONJ associated with oral bisphosphonates, and the first one was in Australia, where oral surgeons identified cases prospectively. The percentage of patients with BIONJ (who had taken an oral bisphosphonate) was five- to tenfold greater than reported in other case studies to date.3 In a recent U.S. large institutional study, researchers identified 208 patients with a history of alendronate use. Nine out of 208 had active BIONJ and were being treated in the institution’s dental clinic. Approximately one in 23 of these patients were receiving alendronate (which equals about 4% of the population).8
According to a 2006 study in the New England Journal of Medicine, estimates of incidence of BIONJ at that time were based on unsubstantiated claims, and there is general agreement on the need for well-designed prospective cohort studies.8 Better designed prospective cohort studies should help determine more reliable estimates of BIONJ incidence.
Infection and BIONJ
BIONJ case studies have revealed the consistent presence of biofilm infection and pain.3 A variety of bacterial species have been implicated, and in many cases, histology reveals the presence of actinomycosis and mixed bacteria.9 One study retrospectively compared 178 patients with multiple myeloma to determine if antibiotic prophylaxis before dental procedures prevented BIONJ. Most of the patients received intravenous bisphosphonates (in the form of zoledronic acid) at hematology centers.
Data analysis focused on the correlation between dental procedures, antibiotic prophylaxis, and BIONJ occurrence. Dental procedures were more frequent compared to the general population because patients with multiple myeloma are more susceptible to dental ailments. About 75 patients received at least one dental procedure, and 43 patients received antibiotic prophylaxis. Eight cases of BIONJ were recorded, and all eight were in the group of patients without antibiotic prophylaxis. The researchers speculated that antibiotic prophylaxis might prevent BIONJ occurrence after dental procedures. Evidence linking antibiotic prophylaxis and BIONJ prevention is weak but intriguing as an early theory.
I.R. Reid of the Osteoporosis Research Center at Creighton University postulated that the development of biofilms in BIONJ lesions is the result of the local environment and the lesions being chronic. He also mentioned the possibility that the presence of bisphosphonates on the bone surface facilitates their development. Biofilms may also be a major factor in bone resorption despite the presence of bisphosphonate in bone, because bacteria have been shown to stimulate bone resorption.3
Identifying At-Risk Patients
How does an RDH identify patients at risk for BIONJ and how should these patients be managed?
In today’s busy dental practices, it’s easy to overlook a patient’s medical history, especially when seeing patients for recare. It’s important to identify those patients who take bisphosphonates or who have a history of bisphosphonate therapy, and this may require a concerted effort on the part of the entire dental team. New and recare patient histories should include questions about osteoporosis and osteopenia medications, both past and present. It’s easy for patients to forget to disclose their bisphosponate use because some, like Boniva®, Actonel and Reclast®, are not taken daily.
It’s important for oral health-care professionals to determine an appropriate communication protocol with oncology patients that includes not only how to protect the patient’s oral health during cancer therapy, but also a history of intravenous bisphosphonate therapy. Dental treatment should be scheduled in consultation with the patient’s oncologist, and it’s important to ask if the patient received intravenous bisphosphonate therapy and for how long. Common intravenous nitrogen-containing bisphosphonates include pamidronate (Aredia®) and zoledronate (Zometa®).
It’s important to separate patients with osteopenia or osteoporosis who are prescribed an oral bisphosphonate, from those patients who are taking or have taken an oral bisphosphonate. Robert Marx, Joseph Cillo, and Juan Ulloa, Division of Oral and Maxillofacial Surgery at the University of Miami Miller School of Medicine, report that patients taking oral bisphosphonates for less than three years have little risk for osteoporosis. Therefore, the dental team can work with patients in this category to establish optimum oral health and repair the dentition. Nonrestorable and abscessed teeth should be removed first, followed by periodontal therapy and an established recare regimen. Root canal therapy and restorative procedures, including prosthodontic appliances, can follow. Dental implants will osteointegrate during this period, and little is known yet about orthodontic care.
Patients who present for dental care who have used oral bisphosphonates must be asked how long they used oral bisphosphonates, dose, indications for use, and any use of concomitant steroids or other medications that could affect bone healing. For patients who used oral bisphosphonates for less than three years, bone healing should be uncomplicated. If a patient reports three years or more of oral bisphosphonate use or use with concomitant corticosteroid or chemotherapy, some experts recommend a serum CTX test. The serum CTX test is a bone turnover marker that assesses risk and guides a clinician’s treatment planning for certain surgical and non-surgical procedures.10
Don’t dismiss a patient’s comments about pain in the jaw, especially if there is a history of bisphosphonate use. Oral health-care professionals will examine both intravenous and oral bisphosphonate users, and it’s important to know how long the patient has been taking the drug. The longer someone has been on the drug, the greater the risk for BIONJ.4
Supervising patients at risk for BIONJ has many management aspects, so it’s best to read and study the American Dental Association (ADA) recommendations for handling these patients. The ADA Council on Scientific Affairs updates these recommendations regularly at http://www.ada.org. In addition, oral health-care providers should read the best available published data and opinions of national BIONJ experts as the scientific community continues to grapple with this uncommon and puzzling condition.
Author’s acknowledgment: I thank Dr. Robert Marx for reviewing this manuscript. Dr. Marx was the first oral surgeon to describe BIONJ in dental literature.
References
- Munn N, Collinson D. Lighting up darkest. On Fire Mission and Ministry Jan 19, 2008. 9(1): 6-8.
- Marx RE. Uncovering the cause of “Phossy Jaw” circa 1858 to 1906: oral and maxillofacial surgery closed case files — case closed. J Oral Maxillofac Surg 2008. 2356-2361.
- Reid IR. Osteonecrosis of the jaw — who gets it and why? Bone 2008; doi: 10.1016/j.bone.2008.09.012.
- Stadeker WJ. Bisphosphonates 101: an update for the general dentist. Inside Dentistry Oct 2008: 2-6.
- Khan AA, et al. Canadian consensus practice guidelines for bisphosphonate-associated osteonecrosis of the jaw 2008; J of Rheumatol; 1391-1397.
- Edwards BJ, Migliorati CA. Osteoporosis and its implications for dental patients 2008; J of Amer Dent Assn; 139: 545-551.
- Khan AA, et al. Bisphosphonate-associated osteonecrosis of the jaw 2008. Internet. Final proof of systematic review. Available at http://www.caoms.com. Accessed Mar 23 2009.
- Sedghizadeh PP, et al. Oral bisphosphonate use and the prevalence of osteonecrosis of the jaw — an institutional inquiry. J Am Dent Assoc 2009; 140: 61-66.
- Montefusco V, et al. Antibiotic prophylaxis before dental procedures may reduce the incidence of osteonecrosis of the jaw in patients with multiple myeloma treated with bisphosphonates. Leukemia & Lymphoma 2008; 49(11): 2156-2162.
- Marx RE, Cillo JE Jr., Ulloa JJ. Oral bisphosphonate-induced osteonecrosis: risk factors, prediction of risk using serum CTX testing, prevention, and treatment. J Oral Maxillofac Surg. 2007 Dec; 65(12): 2397-2410
About the Author
Lynne Slim, RDH, BSDH, MSDH, is an award-winning writer who has published extensively in dental and dental hygiene journals. Lynne is the CEO of Perio C Dent, a dental practice management company that specializes in the incorporation of conservative periodontal therapy into the hygiene department of dental practices. Lynne is also the owner and moderator of the periotherapist yahoo group: www.yahoogroups.com/group/periotherapist. She can be reached at [email protected] or www.periocdent.com.