Anesthesia failure, a lack of total and profound anesthesia, is a common occurrence in the provision of local anesthesia delivery. Additional time and alternative delivery techniques are required, and patients may lose confidence in the provider’s skill. This is frustrating for the clinician, and can diminish his or her confidence in the delivery of traditional anesthetic techniques.
Specifically, dental practitioners continually report widespread challenges with successful pain control in the mandibular quadrants. The most widely utilized injection technique is the inferior alveolar nerve block, in which a high-level understanding of anatomical considerations may not be enough to ensure adequate pain control for the dental patient.1 Rest assured, there are several alternative techniques available for the dental provider that require minimal anatomical considerations, demonstrate greater success, or simply require easier technique modifications when compared with that of the inferior alveolar nerve block.
When it comes to their mandibular injection techniques, clinicians must stay SHARP to ensure adequate pain management for the patient. SHARP is a helpful memory tool standing for situation, helpful landmarks, anesthetic volume, relative considerations, and procedure. This applies not only to the inferior alveolar nerve block, but also to the alternative mandibular injection techniques, including the Gow-Gates, Vazirani-Akinosi, and mylohyoid nerve blocks.
This article assists clinicians in SHARPening their skills in reviewing the situation in which the injection is appropriate; helpful landmarks to consider in the delivery of injection techniques; anesthetic volume; relative considerations to integrate with regard to the injection itself; and the injection procedure itself for mandibular injection techniques leading to successful mandibular nerve blockade.
Review of the inferior alveolar nerve block
The commonly utilized method for achieving mandibular anesthesia is the inferior alveolar nerve block (IANB). While the IANB technique may provide adequate results for many clinicians, it also provides several challenges, such as inconsistent anteroposterior location of the mandibular foramen; premature contact with bone (or conversely, the lack of bony contact), bifid, and ectopic nerves; and the requirement of multiple penetrations to achieve profound unilateral anesthesia.
Additionally, published failure rates for the IANB range from 31% to 81% of IANB injections,2 leaving the IA nerve block among the highest of injection failure rates in dentistry.
Generally speaking, providers attempting an IANB reference arbitrary landmarks in identifying a probable location of a nerve that may or may not be present or bifurcated, or provide accessory innervation. Anatomical variances of the patient provide subsequent challenges in the successful delivery of anesthesia via the IANB.
Common challenges with regard to IANB injection technique considerations include premature bony contact and overinsertion or lack of bony contact. If bony resistance is met immediately after penetration, it is likely that the penetration site was either too low or too lateral to the pterygomandibular raphe, requiring the clinician to reinsert at a higher and more medial point along the raphe. Another probable cause is an aberrant lingula.
If bone is not contacted, it is likely that the needle tip is located too far posteriorly (medially). The clinician must withdraw slowly to reposition the barrel more posteriorly over the contralateral mandibular molars until bone is contacted. From a safety concern, depositing solution without bony contact may elevate the risk of approximation of the needle tip in the parotid gland near cranial nerve VII, the facial nerve, in which transient blockade or paralysis of the facial nerve may occur.
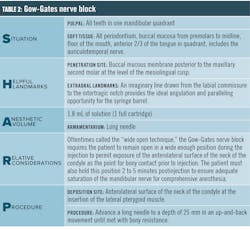
Gow-Gates nerve block
The Gow-Gates nerve block provides anesthesia of the mandibular nerve as it travels through the pterygomandibular space prior to entry into the mandibular canal. Therefore, it anesthetizes not only the inferior alveolar nerve but also the mental, incisive, lingual, mylohyoid, auriculotemporal, and buccal nerves as well as pulpal anesthesia of all mandibular teeth to the midline in one quadrant. This provides multiple advantages, such as requiring only one injection for unilateral delivery, a high success rate, and a diminished potential for postinjection complications.
This injection is contraindicated for patients who are unable to open wide, patients with TMJ disorders and/or trismus, and patients whose large flare of the tragus indicates a wide flare of the condyles and subsequent prevention of the needle from contacting bone prior to anesthesia delivery.
In addition, providers should be cautioned that onset of anesthesia is slower than that of other injections and can take anywhere from five to 10 minutes. Many clinicians new to trying the Gow-Gates nerve block may prematurely deem the injection unsuccessful without waiting the appropriate time to permit adequate saturation of anesthetic to the nerve membrane.
Vazirani-Akinosi closed-mouth mandibular block
In the 1960s, Vazirani published about a closed-mouth technique, and in the 1970s, Akinosi reported an identical technique aiming to achieve successful block of the mandibular division (V3) of the trigeminal nerve. The technique is now named the Vazirani-Akinosi closed-mouth block to honor both doctors who devised and published about the technique.4
The block itself thoroughly anesthetizes the inferior alveolar, incisive, mental, lingual, and mylohyoid nerves with one simple needle penetration placed laterally to the mucogingival junction of the maxillary teeth on the side to be anesthetized. Barrel orientation is considered parallel to the maxillary occlusal plane upon requesting the patient to close after retraction, and depth of penetration is achieved at approximately 25 mm into the tissue for an adult patient. Bevel orientation is the only concern, as it is imperative that the bevel point toward the midsagittal plane (i.e., away from the ramus) to minimize needle deflection during penetration.
The success rate of this injection is about 93%.5 This block technique not only provides adequate anesthesia for restorative, periodontal, and/or surgical techniques of a mandibular quadrant, but also for unilateral temporary motor paralysis for trismus patients with decreased opening capabilities.
Mylohyoid nerve block
In approximately 60% of inferior alveolar injection techniques, accessory innervation to the lingual tissues is provided by the mylohyoid nerve. This overwhelming statistic means that providers who frequently deliver IANBs experience anesthesia failure, not due to poor injection technique but rather due to anatomical considerations.
The mylohyoid nerve is typically anesthetized during the delivery of the inferior alveolar nerve block but is oftentimes obstructed by anatomical landmarks, such as the pterygomandibular fascia or the sphenomandibular ligament.
In addition, the lingual nerve is the most common nerve affected during paresthesia cases, and risk of paresthetic complications increases with supplemental penetrations through and anesthetic saturation of the lingual nerve. Therefore, it is important for providers to consider safety and risks when attempting to achieve supplemental lingual anesthesia in which the provider is attempting to penetrate the IANB region and deliver additional anesthetic within the space housing the lingual nerve.
Providing anesthesia to the mylohyoid nerve effectively blocks sensation to the mylohyoid muscle and the anterior belly of the digastric while certainly providing supplemental anesthesia in common cases of inadequate lingual nerve anesthesia.
With ease of delivery, the mylohyoid nerve block is completed by retracting the tongue (in which this author wishes her colleagues the best of luck) and penetrating below the apex of the most posteriorly placed tooth on the side requiring anesthesia. Upon gentle contact with bone, anesthetic is safely delivered to provide supplemental lingual anesthesia without high risk of failure or complications.
The mylohyoid nerve block is an excellent alternative injection technique for most patients. Of course, moving around large mandibular tori may be the one contraindication to the delivery of this injection.
Conclusion
It should be noted that there are additional alternative mandibular injection techniques beyond those discussed in this article, including but not limited to the Loma Linda IANB, as well as the periodontal ligament injection, intraosseous or intrapulpal injections for single-tooth anesthesia, and the intraseptal technique.
With the widespread challenges surrounding the utilization of the IANB and the ease of technique found in alternative mandibular injection techniques, clinicians across the country are actively seeking new opportunities to serve their patients with more efficient, more profound, and more successful pain management techniques. Stay SHARP, America!
References
1. Malamed SF. Is the mandibular nerve block passé? J Am Dent Assoc. 2011;142 Suppl 3:3S-7S. doi:10.14219/jada.archive.2011.0340
2. Malamed SF. Handbook of Local Anesthesia. 6th ed. St Louis, Missouri: Elsevier; 2013.
3. Gow-Gates GA, Watson JE. The Gow-Gates mandibular block: further understanding. Anesth Prog. 1977 Nov-Dec;24(6):183-9.
4. Haas DA. Alternative mandibular nerve block techniques: a review of the Gow-Gates and Akinosi-Vazirani closed-mouth mandibular nerve block techniques. J Am Dent Assoc. 2011;142 Suppl 3:8S-12S. doi: 10.14219/jada.archive.2011.0341
5. Bassett K, DiMarco A, Naughton D. Local Anesthesia for Dental Professionals. 2nd ed. Boston, Massachusetts: Pearson; 2006.
KATRINA M. SANDERS, MEd, BSDH, RDH, RF, is a clinical dental hygienist, author, and international speaker. She serves as the clinical liaison of hygiene excellence and innovation for AZPerio. Known as the “Dental Resultant,” Katrina consults hygiene departments to optimize metrics and patient excellence. She is the founder, CEO, and keynote speaker for Sanders Board Preparatory, a published author with Dentaltown and Today’s RDH, a columnist and advisory board member for Modern Hygienist and the Dental Academy of Continuing Education, and brand ambassador for Dimensions of Dental Hygiene.