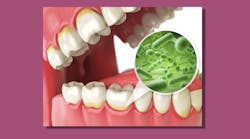
Biofilms are everywhere, in nature and all through the body; some are advantageous and others dangerous. Biofilm in the mouth is a collection of single-celled organisms that live together in a group structure. When all these organisms band together, it changes the way they function they bind to teeth, mucosal surfaces, and dental materials, and cause destruction that they couldn’t do all by themselves.
In recent years, increased understanding of how the oral microbiome impacts systemic health offers newer ways to remove biofilm and combat disease. Guided biofilm therapy (GBT) in particular has emerged as a sound method of biofilm removal on oral surfaces, with many dental professionals considering it a true game-changer in how they practice.
Enjoy (and learn from) our collection of articles on biofilm and guided biofilm therapy: What it is, the risks it poses, and how to help your patients manage it.
Biofilm: Composition and formation
Understanding biofilm and educating patients about the importance of its management, both at home and in the dental office, will help them maintain oral and systemic health. Anne Rice, BS, RDH, CDP, FAAOSH, lays out biofilm’s bacterial composition, the stages of its formation, and some surprising places you could find it other than on teeth.
Biofilm removal for systemic health
Pathogenic bacteria originating in the mouth can set the stage for chronic, degenerative disease. And with compelling scientific data and new advances in dental technology at the forefront, is the dental hygiene profession continuing to use yesterday’s methods to address today’s health issues? Janis Spiliadis, CRDH, and Alisa Cooper, DC, say it may be possible to reduce the risk of developing some cancers by addressing oral biofilms, and offer clear recommendations for both in-office and home care.
The game-changer: Biofilm removal
Guided biofilm therapy: A new protocol with new outcomes
Guided biofilm therapy (GBT) changes the conventional practices of preventive therapy by removing biofilm with air polishing using a low-abrasion powder prior to power and hand scaling. “As a hygienist of many years, I had a hard time wrapping my mind around a new protocol that was different from what I learned in school,” writes Jamie Collins, BS, RDH-EA. But since adopting it, she says, “I have found that patients are very willing and happy with the new treatment outcomes.”
Guided biofilm therapy: A new dental hygiene protocol
GBT, continued: What is it, and why do you need it?
Karen Davis, BSDH, RDH, explains the reasons guided biofilm therapy—which she calls the most revolutionary topic she lectures on for clinicians, students, and educators—is vastly superior to conventional biofilm removal with hand or power instruments. Essentially, GBT involves an eight-step process, capitalizing on the concept that pathogenic biofilm drives oral disease and thus should be removed by clinicians in the least abrasive, most efficient, and most comfortable method achievable.
Guided biofilm therapy: What is it, and why do you need it?
The role of power flossers in biofilm removal
These days, there’s a new level of understanding regarding the complexity of periodontal disease. It is now well accepted that gingivitis and periodontitis are complex biofilm-based infections. Anne Nugent Guignon, MPH, RDH, takes a deep dive into “microbial troublemakers” and how research has shown the effectiveness of using a water-jet oral irrigation device—a power flosser—in combination with a toothbrush to remove biofilm and combat disease.