The A1C score: The A1C score is well within the dental hygiene scope of practice
It's not just a casual conversation. The A1C score is well within the dental hygiene scope of practice
BY Marcy Ortiz, RDH, MEd
Knowing the diabetic patient's HbA1c (A1C) score is a critical part of the medical history questioning. Recently, I asked a diabetic patient about his last A1C score. He did not know offhand, but said he would follow up with his physician as he recently had the blood test. His doctor replied that requesting this information from a dental hygienist is "beyond the scope of their practice."
Beyond our scope of practice?!
The doctor was even reluctant to tell the patient what his score was. Relentless, this patient did get his score and brought it to our attention; it was normal. In terms of comanaging health, this experience shows we have a long way to go in integrating medical-dental relationships. It also shows that not all physicians know the scope of the dental hygiene practice.
-----------------------------------------
Read related articles on DentistryIQ
- Diabetes and oral health: The importance of maintaining optimum oral health
- Help in explaining diabetes: Dental hygienists' role in diabetes education involves looking, listening, and feeling too
- What's new in diabetes research, care, and prevention?
-----------------------------------------
Regardless of this experience, it is important for the patient and the dental team to know each patient's diabetic stability. Evidence-based research shows the bidirectional effect periodontal disease has on diabetes and vice versa. A patient with a higher A1C score (suspect uncontrolled diabetes) may require specialized services, referrals for extractions, or more aggressive periodontal treatment, for example, due to this higher risk factor. This article will explore the bidirectional effects between periodontal disease and diabetes, what an A1C score actually measures, why it is important for dental hygienists to know the A1C score, and how we can empower our patients to better manage their oral health and diabetes.
What A1C measures
The A1C score is a simple blood test that gives the patient an average blood sugar level over a period of time, usually the last two to three months. Physicians use the A1C test to diagnose diabetes, evaluate how a patient is managing the disease, or determine the need to alter the patient's treatment plan, which may require lowering or adding medication.4 The blood test measures the glucose that is attached, or glycated to blood hemoglobin, a protein found inside red blood cells which carry oxygen throughout the body.5 These cells have a life span of three months before they die and regenerate with the corresponding glycated glucose on the cell lasting the same amount of time.5
When taking an A1C score, these cells are evaluated at their three-month capacity for glucose attachment (glycated) to hemoglobin. If there is too much glucose attachment, the A1C score is high; if there is a normal amount of glucose attachment, the A1C score is normal.4
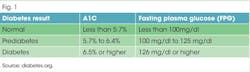
The test results are given in a percentage which determines the stage of health or disease. A lower percent indicates normal or controlled diabetic condition; a higher percent indicates more blood sugar and less disease control or stability, especially when greater than 6.5% (see Figure 1). It is not unheard of for diabetics who have difficulty managing their disease to have an A1C score in the 7.0%-8+% level.
The frequency of an A1C test is conducted depending on the type of diabetes and history of diabetic control for each patient. For type 2 diabetes (no insulin), two times per year is sufficient if past results are stable. Three to four times per year may be necessary for the type 1 diabetic patient or if there is history of glucose instability.6
Bidirectional effects
The bidirectional effect between periodontal disease and diabetes has been extensively studied. Bidirectional means both diseases and their inflammatory factors, when not treated or controlled, directly affect the other negatively. Notably, "periodontal disease makes it more difficult for people who have diabetes to control their blood sugar."1 Diabetic patients have a high incidence of periodontal disease, especially if their diabetes is uncontrolled. Because of this high incidence, it is no surprise that "periodontal disease is often considered a complication of diabetes."1
Illustrating the bidirectional relationship of diabetes and periodontal disease is a heavily studied group of people, specifically 5,000 Pima Indians living on the reservation in Southern Arizona. Genco (2008) reports the Pima Indians are a unique population because they have an "extremely high incidence of type 2 diabetes (40%) and very high levels of periodontitis"; 80% of this population has been studied for more than 25 years, yielding profound systemic results.2
The patients who had diabetes with periodontal infections had worse glycemic control over time, and the periodontal disease was more severe in those who had diabetes compared to those without diabetes.3 Thus, periodontitis made diabetic glycemic control more difficult and was shown to worsen the complications that accompanies their diabetes. However, treatment of periodontal disease had a positive effect on glycemic levels for the diabetic patients.3 This study reinforces the need to treat patients with a cohort of systemic disease differently from the average patient. An uncontrolled diabetic patient who also displays periodontal disease requires aggressive treatment, not only for their periodontal disease but also for the sake of better diabetic glycemic results. This is especially true if these same diabetic patients have higher than normal A1C scores. Comanaging these patients with their physician or endocrinologist is important in reinforcing the importance of stabilizing both diseases and to build a cohesive dental-medical integrative relationship.
Diabetes facts and statistics
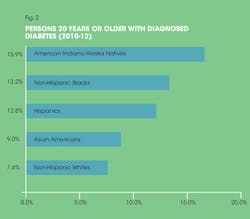
Diabetes affects a staggering amount of the American population. According to the 2014 National Diabetes Statistic report, 29.1 million people in the United States have diabetes (9.3%); diagnosed cases are 21 million with undiagnosed cases estimated at 8.1 million7 (CDC). To break down further depending on race/ethnicity, American Indians/Alaska natives have the highest average incidence of diabetes in the United States and non-Hispanic whites had the lowest (see Figure 2). Individually, American Indians in southern Arizona are noted at 24.1%, whereby the Alaska Natives are lower at 6% with diagnosed diabetes varying depending on region.7 This level for American Indians should come as no surprise in light of the Genco Pima Indian study with their very high diabetes incidence of 40%.
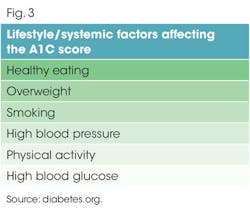
Prediabetes is the condition whereby individuals have a slightly higher A1C level than normal but not to the point of being classified as diabetic. Some patients may still call this "borderline" diabetes. These patients have a high risk of their prediabetes evolving into diabetes if improvement of risk factors is not taken seriously (see Figure 3). Statistically, when including all adult ages, an estimated 86 million Americans are diagnosed with prediabetes based on their A1C level.7 Although this is a substantial figure, prediabetes can be stabilized or reversed to normal. The risk factors of weight and diet play such a significant role in keeping prediabetes stable, they can "prevent or delay type 2 diabetes and, in some cases, return blood glucose levels to within the normal range." 7
Type 1 diabetic patients must have insulin delivered by injection or pump to survive. Diagnosis can occur at any age but peak diagnosis is midteens. Type 2 diabetics are those patients who control their blood sugar with medication or insulin (previously known as adult-onset). This usually occurs later in life, but incidence is starting to rise in younger populations in certain ethnicities such as American Indians, African Americans, Hispanic/Latinos, Asians, and Pacific Islanders.7 Regardless of the type of diabetes, people manage their disease best by including regular exercise, a healthy, balanced diet, and oral medication (or insulin) to lower blood glucose.7
Empowering diabetic patients
Urging patients to understand their diabetic A1C test scores can be critical in getting them involved in their disease control and oral health concerns. Many diabetic patients are aware of the medical concerns, but surprisingly a majority are not knowledgeable about what the A1C scores can mean regarding their oral health. This presents a perfect opportunity to open dialog on the systemic bidirectional capability between periodontal disease and diabetes. If you slowly start having this conversation with your patients, you will be surprised when, upon their next recall appointments, they come armed with their latest A1C score. This patient is now more open about discussing the status of their diabetes because they feel empowered.
When your periodontal/diabetic patients are informed and empowered, they are more likely to accept recommended treatment and recare appointments. Knowing how serious both systemic diseases affect each other can jump-start how proactive your patients are in addressing and managing both diseases. Oral health concerns, along with diet and risk factors, can be discussed with our dental patients at the earliest prediabetes stage, enabling patients to take action in making immediate lifestyle changes.
Most importantly, do not let the condescending attitude of one physician deter your hygienist-patient relationship. Ask for a recent A1C score from all of your diabetic patients and record it in their charts at each visit. We are here to improve our diabetic patients' oral health, which has a significant impact on their diabetes. Having the A1C discussion is an integral part of a thorough medical history, and it is not beyond the scope of our practice. RDH
Marcy Ortiz, RDH, MEd, has been a practicing clinical dental hygienist since 1987, the majority of her time spent working in a geriatric practice in Sun City West, Arizona. She is an adjunct instructor at Phoenix College, Department of Dental Hygiene in Phoenix, Arizona, and a member of Camelback Toastmasters, earning her Distinguished Toastmasters (DTM), the highest communication/leadership award in Toastmasters. Ms. Ortiz is proud of recently cofounding a dental hygiene study club called HART: Hygienists at the Round Table. You may contact her by email at [email protected].
References
1. Diabetes and periodontal disease. (2015) American Academy of Periodontology. Retrieved May 22, 2015 from http://www.perio.org/consumer/diabetes.htm
2. Genco RJ. Perio medicine-The future of oral health. Dimensions in Dental Hygiene. 2008;6(3):16-18.
3. Genco R. What the future may hold: Robert J. Genco, DDS, PhD, discusses the future of oral/systemic links-from pancreatic cancer to Alzheimer's disease. Dimensions of Dental Hygiene. 2010;8(3):22-24.
4. Chung B. (2015). Ask the expert: A1C an important tool in controlling diabetes. Banner Health. 2015;4(1):19.
5. A1C and eAG, (2014). Retrieved May 22, 2015 from www.diabetes.org
6. Tests and Procedures: A1C Test. (2013). Retrieved May 22, 2015 from www.mayoclinic.org
7. Centers for Disease Control and Prevention (CDC). National Diabetes Statistics Report:
Estimates of Diabetes and Its Burden in the United States. 2014; Atlanta GA: U.S. Department of Health and Human Services. Retrieved June 3, 2015 from http://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf.