One heart at a time: Networking leads to discussion about atrial fibrillation and impact on lives
By Anne Guignon, RDH, MPH, CSP
A few months ago, seven inches of rain fell in less than five hours at my house. This kind of rainstorm is not uncommon in Houston. Streets will be flooded for hours following that kind of deluge. Despite the risk of impassible streets, my husband, Derek, and I embarked on the safest route to Memorial Hermann Memorial City Medical Center. It was a tense 10-minute drive. We were laser-focused on ending his three-year battle with atrial fibrillation (AFib), a dangerous cardiac condition that, left untreated, can lead to a stroke or eventually heart failure.
Even though he lost weight, adopted a low-sodium diet, learned relaxation techniques, took a minimal amount of medication, and recognized that sleep apnea was a contributing factor, the threat of landing in the emergency room with another AFib episode or suffering a debilitating stroke kept his life on edge. Surgery was the next step.
Derek had chosen to have the Wolf Mini-Maze minimally invasive cardiac surgery, and we had to be at the hospital by 5:00 a.m. Most streets and freeways were impassible, and the surgeon’s route was flooded; however, the surgery was not postponed. We had to wait. When his doctor, Randall Wolf, MD, arrived, Derek quipped, “Thanks for getting here in your kayak.” Dr. Wolf laughed, and the hospital staff quickly set things in motion.
How Derek and I arrived at this choice for treating his AFib was nothing short of a series of miracles that started three years earlier.
Imagine a conference, not related to health care, with a total attendance of 1,500 people. What are the odds of sitting next to the one person at the event who could help save your spouse’s life? That is exactly what happened in San Diego in 2014 when I met Mellanie True Hills at the National Speakers Association meeting. That weekend was the beginning.
Mellanie had suffered from AFib for years. She knew firsthand how this cardiac condition could quickly consume a person’s every waking moment. After recovering from successful AFib surgery, Mellanie switched her focus in life. She founded StopAfib.org, an organization focused on providing quality information for patients and families about AFib and treatment alternatives. Three years ago, StopAfib.org hosted its first patient-centered conference.
Last year, Derek and I attended the event. It reminded me of RDH Under One Roof. Cardiologists, electrophysiologists, and cardiothoracic surgeons shared information with patients about dealing with AFib. Patients and family members spent time with corporate sponsors supporting the event. We listened to presentations, shared stories with other AFib patients and their families, and spent time learning about various procedures. We also met Dr. Wolf, the developer of the Wolf Mini-Maze surgical procedure who would later become Derek’s doctor. We left the conference knowing the direction we would take.
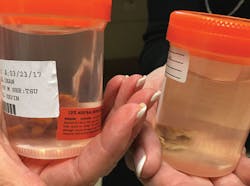
This surgery is performed on the outside of the heart. Heart surgeons use the AtriCure bipolar radiofrequency clamp to create a circumferential scar around the pulmonary veins, which prevents electrical impulses from triggering AFib episodes. The technique also involves removing the patient’s left atrial appendage, a potential troublemaker. Blood can pool in the left atrial appendage and form clots that result in a stroke, so removing it is key. With the appendage gone, the risk of an AFib stroke is nearly eliminated, and patients no longer require blood thinners for stroke prevention.
Over the next few months, Derek took steps to prepare for the surgery. Fortunately, Derek qualified for the Wolf Mini-Maze surgery, which was scheduled for January 18, 2017. During Mass on the Sunday before the surgery, my eyes filled with tears. The enormity of his decision hit me unexpectedly. Derek was having heart surgery and anesthesia. The emotions took me by surprise. Even though I knew Dr. Wolf had performed this surgery more than anyone else in the world and had never lost a patient, there is never a 100% guarantee for any medical procedure. Feeling overwhelmed, I posted my thoughts on my Facebook timeline and asked for prayers. Typically, I don’t put much personal information out online, but this time, I needed support.
Responses started pouring in from dental, business, and professional-speaking friends. This was just the support I needed: hundreds of people praying for a successful outcome. Little did I know, my thoughts would go viral. Readers started sharing links to StopAfib.org and WolfMiniMaze.com. On the day of the surgery, I found a quiet nook just off the waiting room. Friends and family kept tabs on me, and I kept busy reading scientific abstracts and posting updates online. Three hours later, Dr. Wolf came out beaming. The surgery had been successful, and Derek was headed up to the cardiac ICU. Two days later, he was discharged to go home. Over the next couple of weeks, I continued to post updates about his progress online.
Exactly three weeks after Derek’s surgery, a private message showed up from a dental colleague in California. Karen’s husband, Randy, had suffered from AFib since 2009. Over the previous year, he started having episodes three or four times a week. Before reaching out to me, Karen and Randy had a consultation with a well-known San Francisco-area electrophysiologist, who recommended a cardiac catheter ablation and participation in a complex research project. Even though Randy’s quality of life was compromised, neither he nor Karen thought this was the right answer. Randy had his records sent to Houston. He was an optimal candidate for Mini-Maze surgery, which was scheduled for March 23 in Houston.
The emotional impact of any surgery is real. Derek and I had several months to process all of the information. Our questions were answered during an in-person consultation in December. Karen and Randy’s consultation occurred over the phone, and with a great leap of faith, they arrived in Houston two days before his surgery. Knowing that our pre-op experiences could not have been more different, my goal was simply to support Karen and her family. I offered to be at the hospital on the day of the surgery. Karen took me up on the offer.
While Karen and I whiled away the time in the waiting room, we put together the framework for this article. We discussed the power of networking, how information can change lives, and how dental professionals can impact those around them in positive and unexpected ways. From my perspective, the time flew by, but that was not how Karen or her daughter felt. I had walked in those shoes, and I knew the drill. After an anxious wait, a smiling Dr. Wolf emerged with good news. Randy’s surgery was successful, and his left atrial appendage had been removed. It was time to take a deep breath, hug, and let the tension of the day go.
But this is not the end of the story. On the day before Randy’s surgery, I posted a brief note about Karen and Randy on my timeline. People started telling their AFib stories. Sadly, some had lost loved ones, while others had family members who were still grappling with the condition. And the conversation went on. A Houston-area dental hygienist I’ve known for decades shared my posts with her former employer. His wife was scheduled for a cardiac catheter ablation, but after learning there was another option, she rethought her plans and had Mini-Maze surgery instead.
As an educator, I am compelled to tell Derek’s story and weave it into many of my continuing education programs. Treating AFib patients is complicated. Every patient is different; symptoms and triggers vary with everyone. Some people know when they have AFib, and others do not. Some people just live with the condition, while others find the impact on their lives intolerable. Some are unaware of their AFib problem until they have a life-threatening stroke. Derek’s cardiologists had only offered him medications. He learned about cardiac catheter ablation on his own and learned about the Mini-Maze option at the StopAfib Atrial Fibrillation Patient Conference.
We need to step back. All health-care providers have a legal, ethical, and moral obligation to provide information about the risks and benefits of all options - including no treatment. This obligation extends into the dental arena. The parallels between treating people with AFib and treating people with periodontal disease are worth consideration. Both conditions are complex, ongoing, and multifactorial. Neither should be treated with a cookie-cutter, one-size-fits-all approach. You would not want that for yourself or those you care for. Derek’s story is a perfect example of why patients deserve the whole story. Take time to consider the following question: Are your dental patients being given the full range of options or just the treatment your office wishes to provide? And if it’s the latter, what are you going to do about it?
One week after Derek’s surgery, I presented a full-day course minutes from my house. During the break, a hygienist I used to practice with said her husband thought he had AFib. It turns out that he does not, and now he is being evaluated for other heart issues. This was not an isolated incident. Hygienists contact me after every program because they want to know about AFib options. A California hygienist contacted me because she was hoping to share information with patients who have AFib. And a Michigan hygienist, who was feeling desperate, made contact with me after her husband’s second visit to the emergency room in nine days.
Despite what many people think, dental hygienists are not “the periodic mouth-cleaning crew” that shows up every three to six months to clean up whatever has happened in the interim. We’re specialists in oral medicine. We evaluate patients from head to toe. People want information. They listen to us. We disseminate knowledge, and knowledge is power.
The impact we have on lives keeps getting bigger and bigger. The whole-body health-care message needs to go to a higher level, and the message about AFib is just one example. What are your passions and messages? What do you want your patients to hear from you? Is your passion soft-drink consumption, obstructive sleep apnea, erosion, obesity, tobacco, or vaping?
Pick a message that resonates with you and share it with your patients. We’re not just about teeth - we’re about people. RDH
ANNE NUGENT GUIGNON, RDH, MPH, CSP, provides popular programs, including topics on biofilms, power driven scaling, ergonomics, hypersensitivity, and remineralization. Recipient of the 2004 Mentor of the Year Award and the 2009 ADHA Irene Newman Award, Anne has practiced clinical dental hygiene in Houston since 1971, and can be contacted at [email protected].
AFib 101: Taking charge of the future
What is atrial fibrillation?
- An irregular heartbeat, a rapid heartbeat, or a quivering of the upper chambers of the heart
- A malfunction of the heart’s electrical system
- The most common heart irregularity, or cardiac arrhythmia
Prevalence and economic burden in the United States population
- Affects more than 5 million Americans
- Expected to affect 17 million Americans by 2030
- Causes 350,000 hospitalizations annually
- Causes symptoms, which vary widely, in approximately two-thirds of those affected
The odds
- Four times increased risk of AFib for those over the age of 40
- Five times increased risk of stroke for those who have AFib, with 15% to 20% of all strokes occurring as a complication of AFib
- Risk of heart failure and dementia
Action plan
- Discuss all treatment options, risks, and benefits
- Patients must do their homework to find the best treatment
- The Atrial Fibrillation Patient Conference is scheduled for August 4-6, 2017 (getinrhythm.com)