When periodontal breakdown occurs before adulthood, the dental hygienist must be alert in diagnosing disease
Timothy J. Hempton, DDS,
Esther Wilkins, RDH, DMD,
Diane Lancaster, RDH
Often, the public`s perception is that periodontal disease is a natural event in the course of adult life. An old-time expression referring to aging was, "getting long in the tooth." Teeth will appear longer when attachment loss occurs, resulting in root exposure or gingival recession.
Attachment loss, however, is not limited to the adult population. Dental hygienists provide treatment to patients of all ages. Being vigilant to the development of periodontal breakdown is equally important for young patients.
One form of early-onset periodontal disease is known as localized juvenile periodontitis. Juvenile periodontitis typically may be first observed in individuals around puberty, ages 11 to 13. The two forms of juvenile periodontitis are generalized and localized. The localized form has characteristic clinical features.
Localized juvenile periodontitis is not a common finding in clinical practice. However, it does have a significant prevalence in the population. In the United States, the highest prevalence of localized juvenile periodontitis is among the African-American population. Females may be more susceptible than males.
Clinical characteristics
Deep pockets of localized juvenile periodontitis are typically observed around the first molars and incisors, both maxillary and mandibular. The most unusual feature of early juvenile periodontitis is a lack of gingival inflammation, particularly around the areas with deep probing depths.
A 14-year-old African-American female who was diagnosed with localized juvenile periodontitis can be seen in figure 1. Observe that there is no apparent gingival inflammation. The supragingival plaque score for this patient was low. Supragingival and subgingival calculus accretions were not detected. Minimal or no inflammation (as well as little or no calculus) is a clinical finding that is very common for patients who are in the early stages of localized juvenile periodontitis.
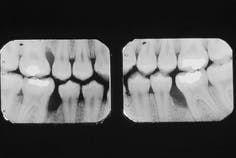
Bitewing radiographs for the 14-year-old patient can be seen in figure 2. Severe vertical loss of alveolar bone on the mesial aspects of the mandibular right and left first molars and the maxillary right first molar is evident. Bone loss localized to the first molars and incisors is characteristic of this disease entity. The image seen on the radiographs is typical of localized juvenile periodontitis.
Note that, although three of the first molars are affected, no significant bone loss can be seen on the adjacent posterior dentition. The maxillary left first molar is not affected in this case. Previous clinical investigators of localized juvenile periodontitis have reported that bone loss does not always occur on all four first molars. In addition, the incisors are also not always affected.
Actinobacillus actinomycetemcomitans (Aa) is the bacterium most commonly associated with this disease. The bacteria are often isolated from the subgingival, loosely adherent plaque inhabiting the pockets associated with the severe bone defects.
The rate of bone loss in localized juvenile periodontitis is about three to four times faster than in chronic adult periodontitis. It is because of this rapid deterioration that the dental team must be careful to properly monitor all patients, particularly the young. The aggressive periodontal breakdown caused by this disease can result in loss of the patient`s maxillary and mandibular first molars and incisors at quite an early age.
Treatment for localized juvenile periodontitis
If the disease process is observed at a very early stage, treatment can include subgingival scaling and root planing in conjunction with antibiotic therapy. The bacteria associated with this disease process are particularly susceptible to antibiotics such as tetracycline or doxycycline. Short-term antibiotic therapy in conjunction with non-surgical treatment can have a significant impact on the loosely adherent flora. Conservative therapy may arrest the periodontal breakdown.
If conservative treatment does not result in a resolution of the disease process, the therapist may switch to surgical therapy. The treatment would include flap elevation of the affected areas followed by thorough root debridement. Commonly, a bone graft procedure such as osseous regenerative therapy is used to treat the lesions.
Today, therapists can place bone graft materials in conjunction with membranes used for guided tissue regeneration. The membranes are used during these procedures in order to enhance the formation of new attachment to the treated root surface. Resorbable or non-resorbable membranes are now available. When surgery is performed, adjunctive antibiotic therapy is usually employed.
The 14-year-old female discussed in this article was treated with bone graft procedures in her mandibular right and left and maxillary right posterior sextants. Tetracycline therapy was also prescribed.
Surgical exposure of her mandibular right first molar can be seen in figure 3. Note that the lesion is limited to the mesial aspect of the first molar. The bone height is completely intact on the distal aspect of the second bicuspid. The type of intrabony defect present in this photograph is known as a three-wall defect, and it is very amenable to bone-grafting procedures.
Granulation tissue had been removed from the intrabony lesion prior to taking the photograph. However, no root planning had been performed. Note that mineralized accretions are not evident on the mesial aspect of the mandibular molar adjacent to the bony defect.
Calculus is not typically observed on the root surfaces adjacent to the bone defects associated with localized juvenile periodontitis. This is in contrast with the deep intrabony defects that can occur in patients with adult periodontitis. Minerals that compose the calculus do not cause bone loss, but the accretions have rough surfaces which are bacterial or plaque retentive.
Plaque bacteria are generally accepted to be responsible for the initiation of the destruction of the alveolar bone and the other tissues that form the attachment apparatus. The plaque-retentive feature of calculus may not be necessary to facilitate the growth and activity of the aggressive bacteria associated with localized juvenile periodontitis.
Host or immune factors
White blood cells play an important role in protecting a patient from bacterial infections. All forms of periodontal disease are bacterial infections. When a patient`s immune system is impaired, the host response to invading bacteria may not be effective.
White blood cells, the neutrophils, function as the first line of defense in infected tissues. In acute infections, they are the predominant cells found in purulent exudate or "pus." The immune cells move toward the bacteria that have invaded the gingival tissues, engulfs the bacteria, and destroys the foreign cells.
A number of researchers have documented that patients with localized juvenile periodontitis have impaired neutrophils present in their periodontium. These defective white blood cells may not respond quickly to bacteria that have entered the periodontal tissues. In addition, the neutrophils may have a weakened ability to engulf and digest the microorganisms. The host defect, present in patients with localized juvenile periodontitis, could account for the rapid and extensive tissue destruction initiated by plaque bacteria.
The disease process may have a genetic component. If, during the examination of the patient, localized juvenile periodontitis is recognized, it would be of value to discuss the findings with the patient`s parents as well as the patient. If the patient has siblings, they may also have this condition.
Advising the patient`s parents can provide the opportunity for examination of the siblings so that a periodontal assessment can be provided. In addition, information about the possibility of a genetic linkage to localized juvenile periodontitis can be explained to patients (who may be teenagers), so that they can be aware that the condition could be passed on to their future children.
Localized juvenile periodontitis is a periodontal condition that is usually detected in individuals around the time of puberty. The dental hygienist must always be aware that periodontal disease is not necessarily an "adult" disease process. After recognizing that children and teenagers may be susceptible to early-onset periodontal disease, the hygienist must be constantly on the alert for the detection of periodontal breakdown. When localized juvenile periodontitis is detected, therapy must be initiated as soon as possible, since the rate of breakdown is much more rapid in this disease process than in adult periodontal disease.
Timothy J. Hempton, DDS, and Esther Wilkins, RDH, DMD, are members of the department of periodontology at Tufts University School of Dental Medicine. Diane Lancaster, RDH, is a practicing hygienist in Dedham, Mass.
Figure 1: A 14-year-old African-American female diagnosed with localized juvenile periodontitis.
Figure 2: Bitewing radiographs of the patient reveal severe bone loss on the mesial aspects of teeth #3, 19, and 30.
Figure 3: Surgical exposure of the bony defect on the mesial aspect of tooth #30.