Note the grand scale of bleaching
Howard E. Strassler, DMD, FADM,
Sheryl E. Syme, RDH, MS,
Jacquelyn L. Fried, RDH, MS
Consumers may perceive tooth whitening as merely any procedure or product that will make smiles "white and bright." Store shelves contain numerous whitening toothpastes and over-the-counter bleaching products. However, both over-the-counter and professionally applied systems are available options to consumers wishing to improve the esthetic appearance of their teeth.
Until 1989, dental practitioners offered only limited treatment options for esthetically improving the dentition`s appearance. Most involved invasive restorative procedures such as esthetic bonding with either composite resin or porcelain veneers, ceramic crowns, or porcelain-metal crowns.
Of all the esthetic restorative treatments performed by dental practitioners, tooth bleaching is the most conservative. In the early 1990s, there were limited choices for tooth-bleaching products. Most products were 10 percent carbamide peroxide gels. Today, dental professionals have more bleaching products and technique choices available to them. The latest vital tooth-bleaching materials and techniques afford dental professionals the ability to offer consumers tooth-whitening treatments with minimally invasive procedures.
This article examines the dental hygienist`s role in vital tooth bleaching and in using a variety of techniques and products.
The dental hygienist plays an important role in establishing, managing, and maintaining tooth-bleaching procedures in the dental practice. During the preventive maintenance appointment, the dental hygienist also can introduce or explain the tooth-whitening options available to the inquiring patient. During this visit, the dental hygienist may also field patients` questions about the effectiveness of different whitening systems to prolong or improve the perceived "whitening" result of the professional prophylaxis.
The refinement of bleaching products
Many techniques are available for tooth whitening. A once popular technique involved hot bleaching with a high-concentration (30 percent) hydrogen peroxide. Problems associated with this technique include:
- It could only be performed in a dental office.
- It involved a special heat lamp.
- It usually involved three to five patient visits.
- It required rubber dam placement.
- It was generally associated with tooth sensitivity following the heating of the hydrogen peroxide on the tooth.
Few dental practitioners performed vital tooth bleaching for these reasons.
Subsequently, clinical reports by periodontists revealed that when patients used over-the-counter carbamide peroxide gels for treating gingivitis, there was a tooth-whitening effect. In 1989, a research study was initiated to evaluate the whitening ability of a 10 percent, carbamide peroxide gel. Patients were instructed to place a small amount of the peroxide in a custom fabricated mouthguard and wear it at night. A noticeable whitening effect occurred. Although the gel under study is not marketed for tooth whitening, a variety of other carbamide peroxide products specifically target tooth whitening.
Without the undesirable heating process, the dental profession has become more accepting of vital tooth-whitening systems containing peroxide. The ADA`s Council on Dental Therapeutics evaluated oral hygiene products marketed for their whitening potential. A review of the dental literature reveals more than 200 published articles that address these products. Most attest to the safety and effectiveness of these materials. To date, no long-term adverse effects have been reported.
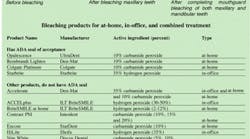
In August 1994, the Council on Dental Therapeutics issued a report on guidelines for safety and efficacy criteria for peroxide-containing products intended to be used for vital tooth whitening. The Seal of Acceptance may be granted to products that meet the criteria and for which safety studies and clinical data from two clinical studies have been submitted, demonstrating at least two value-oriented shade increments of change when the bleaching recommendations are followed.
To date, three mouthguard, vital-bleaching gels have received the ADA Seal of Acceptance. The at-home products are all 10 percent carbamide peroxide gels or pastes. They include Rembrandt (Den-Mat), Platinum (Colgate), and Opalescence (UltraDent).
Wearing a mouthguard at home
The technique for mouthguard vital bleaching requires the least amount of time. It is also referred to as at-home bleaching. Before starting any bleaching procedure, the patient must have a complete oral exam and dental prophylaxis.
The current tooth color provides a baseline for the bleaching process. A standard dental shade guide can be used, and printed shade guides accompany most bleaching kits. A photograph can be used as well.
Steps required for the procedure include:
- Documenting the correct color of the teeth.
- Making alginate impressions.
- Pouring stone casts and trimming.
- Fabricating a mouthguard.
- Mouthguard try-in and trimming.
- Patient education.
Patients may elect to have one or both arches bleached. Accordingly, one or two alginate impressions of the arch or arches are taken. A stone cast then is poured and trimmed with a minimal base so that a vacuum mouthguard can be fabricated. Either a thin or moderately thick, soft mouthguard material is usually supplied with the bleaching kit.
Before fabricating the mouthguard on the vacuum former, a paint-on spacer is applied to the teeth being bleached. The spacer is usually a flowable paste that is light-cured with a composite resin light curing unit. The spacer should be painted on the facial surfaces of the teeth being bleached keeping the material away from the incisal edges, buccal cusps, and cervical margins of the teeth.
Once the mouthguard is vacuum-formed on the stone cast, it is trimmed with scissors to be scalloped to follow the free margin of the gingiva on both facial and lingual surfaces. If the patient has recession on a tooth, the mouthguard should be trimmed to only cover the enamel on the crown of the tooth. Careful trimming of the mouthguard is critical. An overextended mouthguard can cause gingival ulceration where it is rubbing the attached gingiva. The overextension requires additional trimming.
If the tray is not vacuum-formed to the cast correctly, the mouthguard may fit very loosely. In these cases, remake the mouthguard.
Next, the mouthguard needs to be tried in. The dental hygienist evaluates the need for additional trimming of overextensions and rough areas of the mouthguard. This try-in appointment also allows patients to demonstrate their ability to put the mouthguard in and out of the mouth.
In addition, the patient is shown how to apply the bleaching gel into the mouthguard and where to place the gel. Have patients put the gel-containing mouthguard in their mouths. After mouthguard insertion, patients should demonstrate the use of a moist, soft-bristled toothbrush to brush away excess bleaching gel.
Patients are given both verbal and written instructions that describe the technique.
Patients may prefer to sleep with the mouthguard and allow the bleaching gel to work overnight. Others may prefer to wear the mouthguard for two hours each day. The longer the mouthguard is worn and the more frequently the gel is replenished the faster the bleaching will occur.
Patients should be scheduled for a 10-minute follow-up appointment in two weeks. The greatest whitening effect usually occurs in two to three weeks for most patients who adhere to the recommended instructions. After completing the first two weeks of the treatment, patients continue bleaching for another two weeks to see if any additional bleaching effects have been achieved.
As with any technique, adverse reactions have been reported. Patients need to be given instructions in case problems develop. Although adverse reactions have been small in number, the dentist and dental hygienist need to address these issues prior to onset of treatment.
Dislikes of the taste associated with earlier, unflavored products were reported frequently. Since most of today`s mouthguard bleaching gels are usually mint flavored, taste complaints are virtually non-existent.
Additionally, patients may report an increase in tooth sensitivity when using any bleaching product. However, this reaction is seen more frequently with the carbamide peroxides containing higher concentrations (15 to 22 percent). Sometimes merely changing brands is sufficient to stop the problem. If the patient applies a potassium-nitrate desensitizing toothpaste in the mouthguard (before bleaching for 10 minutes), the sensitivity often decreases. Subsequently, the patient should then clean the mouthguard and continue with the bleaching regimen.
Another problem sometimes experienced is a change in the gingival tissues. The gingiva may turn white adjacent to the mouthguard due to a bleaching effect of the soft tissue. This temporary condition will go away within an hour after the mouthguard is removed from the mouth. Some reports suggest that carbamide peroxide gels actually lead to healthier gingiva since they were initially used for the antiseptic treatment of gingivitis.
A sudden blitz at the office
In-office bleaching is beneficial for a motivated patient who will not or has not been able to comply with a mouthguard regimen for at-home use. Appointing the patient for five consecutive days for 20 minutes each day using the mouthguard has been successful in whitening the teeth.
Concerns about high-concentration aqueous hydrogen peroxide (30 percent), heating the teeth, and the extensive regimen required for in-office bleaching caused this technique to come into disfavor. Subsequently, a 35 percent carbamide-peroxide gel (QuikStart, Den-Mat) was introduced.
The gel formula did not have any of the problems associated with the hydrogen peroxide liquid. It was safer for soft tissues and did not require placement of a rubber dam. Isolation was accomplished with a blue-colored, light-curing flowable paste or it could be used in a mouthguard similar to the one used for at-home bleaching.
It has been shown that heating the 35 percent carbamide peroxide to 140 degrees F in its syringe and then applying it to the teeth for 10 minutes at a time enhances the effect of the higher-concentration gel without heating the enamel directly. The authors heat the syringe either using a hydrocolloid impression water bath or by customizing a plastic food storage container, cutting holes in the top (to hold the bleaching syringe) and heating the water in a microwave before immersing the syringes to heat the 35 percent carbamide peroxide.
Another manufacturer, UltraDent also has introduced a 35 percent carbamide peroxide bleaching gel (Opalesence Quik). In most cases, this in-office procedure takes two to three visits to see a five- to seven-value shade change.
Another technique for in-office bleaching uses a light-activated 35 percent hydrogen peroxide bleaching agent that is mixed with an activation powder forming a paste and requires rubber dam placement. The paste is applied and reapplied to each tooth to be bleached and exposed to a curing light for one to three minutes per tooth. Although the technique is successful, it is no more successful than the more ready-to-use 35 percent carbamide peroxide gels.
When light curing over extended periods of time (20 to 30 minutes for an arch from canine to canine), multiple lights must be used to avoid overheating the light curing unit and causing potential damage to the light. This technique is best used when one or two teeth need bleaching. Although one visit of multiple treatments can be successful, usually two to three visits will give the most optimal results.
All hydrogen peroxide in-office bleaching products require the use of a rubber dam to avoid soft tissue damage that may occur due to direct contact with the hydrogen peroxide.
Other treatment options
For many patients, waiting two to three weeks to see a change in appearance of the teeth is a long period of time. Patients may require a technique that produces more immediate results.
Recently, a bleaching system (Accelerate, Den-Mat) was introduced, which uses a combined bleaching kit that contains an in-office 35 percent carbamide peroxide agent (Accelerate Chairside) and the companion at-home bleaching system. The clinical technique requires one week of treatment. On the first day, a 20 to 30 minute session of in-office bleaching as previously described is followed by six days of at-home mouthguard bleaching.
When the patient returns in one week, the in-office treatment is repeated. A Tufts University School of Dental Medicine study reported on an average of seven shade changes and up to 13 shades in some cases after one week of this treatment.
The newest form of bleaching utilizes either one or two different types of lasers. While it has been heralded as the fastest bleaching system, no clinical data validates this claim. Of all bleaching methods, it is the most expensive - almost four to six times more costly - yet it appears to achieve the same end result.
The American Dental Association recently expressed the need for more scientific information to document the use of lasers for bleaching. Reports have been limited to the media and advertising. At this time, not enough information is available to endorse this type of bleaching.
Maintaining the whiter look
For those patients who have been successfully treated with bleaching, maintaining that esthetically pleasing appearance is important. The ADA guidelines for bleaching products with the ADA seal requires that the products demonstrate after six months that the whiter color is still present.
It is important that patients with known oral habits that can cause staining of the teeth (use of coffee, tea, cola beverages, and tobacco products) be advised to use a whitening toothpaste that has a known low abrasivity. Whitening toothpastes may play an important role in maintaining the patient`s whiter teeth after they have completed their tooth-bleaching treatment.
While many toothpastes make claims of stain removal, the dental hygienist should request manufacturers` clinical evidence that the whitening toothpaste does what it claims to do. These toothpastes may work best with powered toothbrushes because the mechanical action of these brushes involve many more strokes per minute than manual brushing can deliver.
Furthermore, patients should be advised as to the detrimental effects of their oral habits, particularly the potential of tooth staining. Long-term bleaching results can be negated because of the return of the discolorations.
References available on request.
Howard E. Strassler, DMD, FADM is a professor and director of operative dentistry at the department of restorative dentistry, University of Maryland Dental School. Sheryl E. Syme, RDH, MS, is an assistant professor in the department of dental hygiene and the school. Jacquelyn L. Fried, RDH, MS is an associate professor in the department of dental hygiene. Request reprints from Dr. Strassler, Dental School, University of Maryland, 666 West Baltimore St., Baltimore, MD 21201; 410-706-7047.
What patients need to know about bleaching
The usual informed-consent procedures and thorough treatment-planning consultations take place prior to initiating tooth-whitening treatment. Whenever a patient selects vital tooth bleaching as a treatment option, the dentition is evaluated for any existing restorations.
In most cases, all anterior composite resins are replaced at the completion of the bleaching treatment. The peroxide bleaching gels cannot change the color of the composite resin. While the teeth get whiter, the composite resin restorations remain the same color as the teeth used to be. In addition, some bleaching gels can cause a change in the hardness and surface of composite resins.
Patients need to understand these changes. They will want to plan on any additional expenses that will incur during the replacement of the composite resin restorations.
Teeth also can be darker in color or have discolorations that present themselves as white or brown spots for a variety of reasons. Tooth discolorations can be classified according to etiology.
Conditions that can cause tooth discolorations include:
- Enamel hypoplasia due to fluorosis (generally manifested as white, flecked areas or whitish and brown spotting on the enamel).
- Tetracycline staining of the teeth due to the ingestion of tetracycline while the teeth were forming (evident as mild, moderate, or severe, depending on the darkness and banding of the yellow, brown-orange, or blue-gray-brown dentinal discoloration. In some cases, the tetracycline discoloration gives the tooth a banded appearance of yellow-orange bands within the enamel.
- Tetracycline-like staining (grayish-blue color) of teeth after they have erupted into the mouth due to the ingestion of minocycline. The antibiotic is taken for the treatment of acne.
- Trauma to a developing tooth during enamel formation. An example is when the primary tooth is intruded into the forming tooth bud of an anterior tooth and hemorrhage into the area causes blood products to incorporate into the enamel matrix of the forming tooth.
- The darkening or yellowing often occurring as a result of aging. As one ages, the porous enamel surface picks up deep stains of coffee, tea, tobacco, cola beverages, and other stain producing foods and beverages that are ingested. Even the coarsest prophylaxis paste cannot remove these embedded stains. With aging, enamel becomes thinner due to the abrasive action of brushing with toothpaste and acid erosion from ingested foods and beverages. The underlying dentin is yellow-orange in color and it appears to be more prominently displayed once the enamel thins.
The tooth discolorations with the best prognosis for whitening are the yellowing of the teeth without any systemic or developmental cause. A routine treatment regimen can be enough to change the tooth color by at least two shades and, in some cases, as many as 12 shades.
Recent reports also show that fluorosis staining, darkness of the tooth due to trauma, and tetracycline staining can be treated with vital tooth bleaching. But the time of treatment may need to be extended.
For a patient with tetracycline discolorations, mouthguard bleaching may take three to six months of wearing the mouthguard every night to effect the greatest change. The results may not be as dramatic as for those with yellow-orange discolorations due to deep enamel staining, but for many it will produce satisfactory esthetic change.