Allergic reactions to dental materials, drugs require an alert response from practitioner
Cynthia R. Biron, RDH
An allergic reaction is the medical emergency that can make the most noticeable changes in a patient`s appearance in a matter of minutes. The reactions range from mild rash to a combination of the most serious manifestations of anaphylaxis. In generalized anaphylaxis, the patient can be clinically dead within minutes from the onset of manifestations. Manifestations include urticaria (hives), swelling of tongue, pharynx, larynx, bronchospasm, hypotension, cardiac arrhythmias, and abdominal pain.
Two different cases of allergic reaction that actually happened in dental offices are described here. The names of the patients and the dental team members have been changed to provide confidentiality.
Case 1
Jennifer, a 16-year-old female, was a new patient in Dr. Robertson`s office. She needed an appointment right away since she had fractured tooth #8, and it was extremely sensitive to temperature changes.
Her medical and dental histories were unremarkable, and she had never had restorative dentistry in her life. She had not been to the dentist in eight years and, fortunately, she had no carious lesions or periodontal problems.
Dr. Robertson completed an oral examination and two radiographs. He restored tooth #8 with two pins and composite material. Jennifer was then rescheduled with the hygienist for a prophylaxis and a panoramic radiograph.
When Jennifer returned for the appointment, Allyson, the hygienist, asked if Jennifer had any problems with the tooth that was restored. Jennifer said, "No. The tooth didn`t bother me, but my lip swelled up and was quite fat all night."
Allyson replied, "It was probably irritated from being stretched out during the procedure." She washed her hands and slipped on her rubber gloves. She proceeded to retract Jennifer`s lips and cheeks to look into her mouth. Within seconds Jennifer`s lip began to swell, and her face and neck was covered with red blotches.
Allyson summoned Dr. Robertson. He sensed the urgency in her voice and appeared within seconds. By now, Jennifer had a swollen tongue, and the red blotches were raised into hives. She began to panic and demonstrate difficulty with breathing. Dr. Robertson called for the emergency cart. As soon as it was brought to him, he administered epinephrine by sublingual injection.
He then administered oxygen to Jennifer and requested that Allyson take Jennifer`s vital signs. Allyson stated that Jennifer`s blood pressure was only 80/50. Dr. Robertson placed Jennifer in a Trendelenburg position and increased the oxygen flow rate by delivering the oxygen by non-rebreather bag. Five minutes later, Jennifer began to show an improvement in breathing, and her blood pressure was now up to 130/80. Her baseline blood pressure was 100/70. The sudden increase from the hypotension of allergic reaction to a blood pressure above baseline was from the vasopressor effects of epinephrine.
Jennifer was transported to a local hospital for evaluation. Later, she tested positive for latex allergy.
The quick response by Dr. Robertson probably saved Jennifer`s life. Studies have shown that up to 3 percent of subjects tested had a reaction to rubber gloves. The reactions were to various ingredients in the gloves and not necessarily to latex.
It is conceivable that similar situations have occurred in other dental offices as most dental team members wear latex rubber gloves during patient care. Unless we have dealt with a situation where a patient reacted to the rubber gloves, we are not likely to ask patients if they are allergic to rubber gloves.
Dr. Robertson did not hesitate to use epinephrine - the one drug necessary for the management of allergic reaction. He knew Jennifer was very young and healthy. She was not taking medications, nor did she have any underlying cardiac conditions. Consequently, the emergency was successfully resolved, and the patient did not experience additional problems.
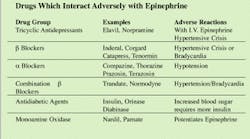
But what about the patients who should not be given epinephrine? They may be taking medications which contraindicate their use, or they have known underlying cardiac conditions or other medical conditions. Such conditions may cause them to be unable to tolerate the effects of epinephrine. The next case is an actual example of an allergic reaction where the dentist did not give the patient epinephrine. He knew the patient was taking an antihypertensive that could cause a hypertensive crisis if taken concomitantly with epinephrine.
Case 2
Douglas Smith, a 35-year-old male patient, presented at an oral surgeon`s office with a history of hypertension that was controlled by the drug Inderal. Inderal is a beta blocker that should not be taken with epinephrine. The combination can cause a hypertensive crisis and/or bradycardia.
Douglas was referred to Dr. Jackson for the extraction of tooth #3. Douglas had a 3 p.m. appointment, and he arrived five minutes before the appointment. The dental assistant, Sheila, seated Douglas and reviewed his medical history and took his vital signs.
When Dr. Jackson entered the room, Sheila told him about the history of Inderal and that Douglas had a blood pressure of 140/90. Knowing that an Inderal blood level contraindicates the use of epinephrine, Dr. Jackson decided to administer lidocaine plain (no epinephrine), for the extraction of the tooth.
The tooth was extracted without complications. But, immediately after the extraction, Douglas began to demonstrate signs of allergic reaction. His lips, oral mucosa, and tongue began to swell, and hives seemed to manifest themselves out of nowhere. His blood pressure and pulse dropped suddenly.
The receptionist was instructed to call EMS, and Dr. Jackson administered Benadryl by intramuscular injection. No improvements occurred, and now Douglas had a blood pressure of 60/40. As unusual as it is for a person to be speaking with such a low blood pressure, Douglas began to blame Dr. Jackson for the reaction, as well as the doctor`s attempts to relieve the symptoms.
When EMS arrived, Dr. Jackson told the paramedics that Douglas was taking Inderal so epinephrine was contraindicated. The paramedics gave Douglas more Benadryl and also cortisone while en route to the hospital. Dr. Jackson rode in the ambulance with Douglas and was subjected to more complaints from Douglas. At the hospital, the emergency room physician administered epinephrine to Douglas, and his condition improved very soon.
Dr. Jackson was still in a quandary as to what could have caused the reaction. Lidocaine is an amide anesthetic and allergies to it are rare. The emergency room staff began to question Douglas about what he ate for lunch. They learned that he had shrimp for lunch. Further testing showed that Douglas was allergic to shellfish, and the allergic reaction just happened to manifest itself at the time of the extraction.
The coincidence is amazing - but not surprising. Allergic reactions don`t promptly manifest themselves all the time, especially if the allergens have not gotten into the circulatory system immediately. Some allergic reactions are delayed for 24 to 48 hours and are termed delayed sensitivity reactions. Had Douglas not presented with a history of taking Inderal, Dr. Jackson would have treated the allergic reaction with epinephrine. Both would have assumed the reaction was from something used in the extraction procedure and not shrimp - unless Dr. Jackson questioned Douglas about what he had eaten before the appointment.
If the cause of the allergy had not been determined, Douglas may have chosen to eat shrimp again and the reaction could have been extreme. Each successive exposure to an allergen intensifies the immunologic response by employing different immunoglobulins. The type 1 IgE response is associated with anaphylaxis. Other reactions in dental offices are less dramatic as they simply result in a rash that is associated with contact dermatitis.
Have a kit ready for the rare emergency
Anaphylaxis is not one of the most common medical emergencies that occurs in the dental office. However, when it does occur, it is going to require the swiftest response. Having a preloaded syringe of epinephrine in the emergency drug kit can save valuable time. No other drug has to be administered as swiftly in an emergency. In addition, no other drug in the emergency drug kit should be in a preloaded syringe as it could lead to confusion in a case of anaphylaxis.
The AnaKit is a beesting kit that is available for allergic reactions. It contains two 50 mg tablets of Benadryl and a preloaded Tubex syringe of epinephrine. The plunger of the syringe is notched to prevent administering the entire contents (1 ml) 1:1,000 epinephrine in one injection. Three doses of 0.3 mls of epinephrine are in the Tubex syringe. With each turn of the plunger, 0.3 mls of epinephrine is delivered through injection.
The sublingual area is the best site for injection of epinephrine with this syringe. The short needle is designed for a subcutaneous injection. Delivering the drug to such a vascular area can produce drug efficacy in five minutes.
The only faster method of delivery is a 1:10,000 intravenous administration. If the patient does not have an IV line already in place, the IV setup for an inexperienced clinician could take longer than five minutes. If the patient is hypotensive, a venupuncture can be a very difficult procedure to perform when veins are collapsed from a fallen blood pressure.
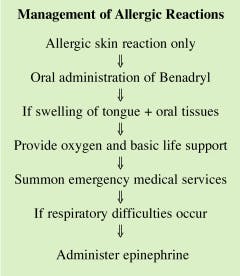
Benadryl blocks histamine release, and cortisone provides anti-inflammatory effects. Benadryl is effective against histamine release and the mild reaction of rash or hives. But it does nothing to block the action of other chemical mediators of anaphylaxis that cause bronchospasm and cardiovascular collapse.
As in the case of Douglas, epinephrine had to be administered to reverse the reaction. When a patient is taking a drug which interacts adversely with epinephrine, the situation is difficult to manage. Another emergency could result from the administration of epinephrine. Dr. Jackson used a conservative approach and kept the emergency under control. If Douglas had begun to experience respiratory depression, epinephrine would have been necessary to restore adequate breathing.
The determining factor is "breathing." If a patient is in respiratory distress, epinephrine must be administered no matter what medication the patient has taken. At that point, if epinephrine is not administered, the patient will die. If breathing is not a problem and only rash and mild reaction are present, oral administration of diphenhydramine (Benadryl) is all that should be done to manage the allergic reaction.
Predisposition to allergic reactions
People with allergies (to pollens, trees, grasses, animals, dust, molds, and medications), a history of hay fever, and asthma are considered to be atopic patients. Atopic patients can be hypersensitive to many products and materials used in dentistry. When taking a medical history, it is very important to document any type of allergy and further question patients about drugs and materials to which they may be hypersensitive. Precautionary measures can be taken if the information is collected in the medical history.
Patients who have never had any allergies or allergic reactions before, though, can suddenly experience a reaction to any drug, product, or material. Anyone can have an allergic reaction at any time.
Adverse reactions to local anesthetics
The most common adverse reaction to local anesthetics is a toxicity reaction, not an allergic reaction. Toxicity reaction is more common when the anesthetic is used plain (without a vasoconstrictor, which prevents the anesthetic from leaving the anesthetized site too rapidly). Amide-type anesthetics have not been a problem in allergic reactions.
Reactions involving amide-type anesthetics have been linked to other products in the anesthetic cartridge, not the anesthesia. Parabens and methylsulfites, for example, are preservatives added to cartridges to prevent oxidation of vasoconstrictors.
Amide-type anesthetics such as lidocaine, mepivacaine, prilocaine, or any generic, amide-type anesthetic can be identified by the presence of two letter (i`s) in the name. Their trade names have one letter (i) such as Xylocaine and Carbocaine.
Ester-type anesthetics can cause allergic reactions. These anesthetics, such as procaine, propoxycaine, and chloroprocaine have the opposite nomenclature in that their generic names have one letter (i) but their trade names also have one letter (i) This makes it difficult to differentiate from amide trade names. Trade names of ester-type drugs are Novocaine, Ravocaine, Nesacaine, and Hurricaine.
Ester-type anesthetics are not commonly used for local anesthesia injections. The exception is for a patient with a liver disorder which contraindicates the use of amide anesthetics. Ester anesthetics are used for topical application for injection sites and scaling sites. Topical anesthetics such as Hurricaine and Solarcaine should be used very sparingly and not allowed to flow into the oropharynx. Excessive amounts or contact with the oropharynx could intensify an allergic reaction.
Drugs commonly prescribed in dentistry
Penicillins containing Amoxicillin - which is used for prophylactic antibiotic against infectious endocarditis - has an incidence of allergy in 7 to 10 percent of the population. Approximately 300 people die each year of anaphylactic reaction due to penicillin. IV administration of penicillin is more likely to cause a severe reaction than oral administration.
Sulfonamides have also been associated with allergic reactions, but other anti-infectives are rarely causes of allergic reaction. Barbiturates have caused allergic reactions, especially in asthmatic patients. Non-steroidal, anti-inflammatory drugs such as ibuprofen have been known to cause allergic reactions in asthmatic patients as do aspirin and other salicylates.
Other allergic reactions to drugs used in dentistry are very rare. Patients often claim to be allergic to codeine since it upsets their stomachs. Unless a patient has experienced skin reactions, swelling and/or breathing difficulties, they have not had an allergic reaction. Reactions to codeine are usually nonallergic gastrointestinal symptoms.
Whenever a patient says they are allergic to a drug, it is important for them to describe the reaction they had to the drug. If true allergic manifestations are not described, they may be alluding to an intolerable adverse reaction that caused them to believe they are allergic. We are not insisting that a patient take a drug causing discomfort. We are trying to determine a patient`s allergic tendencies so that we may avoid similar drugs and prevent allergic reactions.
Other products used in dentistry
Many materials used in dentistry can cause a contact allergy of the oral tissues. Outbreaks may appear as stomatitis where 1 mm red dots are spotted throughout the oral cavity. Or they may appear as aphthous ulcers, erythema multiforme, lichenoid reactions, glossitis, and angioneurotic edema.
Patients who are allergic to rubber (latex) are also allergic to rubber dams and possibly even tubing from blood pressure cuffs and any other form of rubber. Vinyl gloves are an alternative for these patients. Patients who have allergies to shellfish can have an allergic reaction to alginate impression material. Some patients have had minor allergic reactions to prophy paste, mouthwashes, toothpastes, disclosing tablets or solutions, and a host of products used in dentistry. Dental materials causing stomatitis or contact dermatitis include, but are not limited to, amalgam, acrylic, composite resins, nickel in prosthetics, and eugenol.
It is important to remember that allergic reactions worsen rapidly and reverse slowly. Do not hesitate to call EMS. If you call EMS and notice a marked improvement in the patient`s condition, you can cancel the request while they are en route or allow paramedics to evaluate the patient and not necessarily transport the patient to the hospital. It is assuring to know that they are on the way in case the reaction is not reversed or worsens.
We cannot always prevent an allergic reaction from occurring so we must be prepared to manage such an emergency. Epinephrine is one of the most dangerous drugs in the medical emergency drug kit as it could cause a stroke or heart attack if given to a patient with underlying conditions which contraindicate its use. But if you do not have epinephrine available or fail to use it in the case of respiratory depression and/or anaphylaxis, a patient will die.
Take a minute to check the office emergency drug kit. Locate the epinephrine and check the expiration date. If the drug has expired, request a replacement for it. These few actions could save a life since someone took the time to prepare for a life-threatening medical emergency.
Cynthia R. Biron, RDH, is chair of the dental hygiene program at the Tallahassee Community College. She is also a certified emergency medical technician.
Do you have an interesting case?
The Medical Alert column contains actual cases which involved a need for a medical consultation, management of a medical emergency, or a post-op complication. If you know of an interesting and informative case for your readers, please send a brief description of the case to: Cynthia R. Biron, Director of Dental Auxiliaries, Tallahassee, FL 32304-2895. Ms. Biron will contact you for a personal telephone interview. All cases will remain strictly confidential unless a dental team is in agreement with being given recognition for a livesaving medical situation.