Yeah, we know. No one likes the ‘cleaning lady’ stigma. But everyone has to mop a floor, right? Don’t you sweep before you mop?
Many ideas and opinions exist about polishing teeth, including whether or not polishing is a necessary part of a prophylaxis appointment. The American Dental Hygienists’ Association Position Paper on Polishing Procedures states, “Polishing should be performed only as needed and not be considered a routine procedure.”
What about the idea of polishing first? “Pre-polishing” is not a new idea. I first heard of pre-polishing when I worked as a dental assistant between 1987 and 1991. The dentist I worked for had a partner whose hygienist polished first. I remember thinking, “Why does she do that?” I wondered but never asked, partly because I did not have a good understanding of what hygienists do (besides clean teeth and make more money than I did).
I heard about pre-polishing again in March 1994, less than a year out of dental hygiene school, when I attended a continuing education class on insurance codes presented by Kathy Forbes, RDH. Forbes said she polishes first to remove plaque and stain, then there is less plaque to remove with scaling. She made this idea visual by showing a slide of a patient with thick plaque and gingivitis.
I thought, “Aha! So that is why Wendy polished first.”
But I did not run back to my office and pick up the prophy angle first. I work in both the educational and private settings, and the philosophy of selective polishing had been instilled as gospel.
About a year later, I treated the young daughters of a dental colleague and friend of my employer. I was “prepped” by our front office staff that these girls were going to be “tough.” They had a history of negative dental experience, so I was very nervous about impressing my employer by making these girls happy while providing the appropriate care. I had already decided that this was the time to try out the “polishing first thing.”
I sat the oldest girl, 14, in the dental chair and took radiographs, then looked around her mouth with a mirror. I demonstrated sulcular brushing in her mouth with a mirror, then had her go to the sink and brush all her teeth. I supervised and provided feedback, then gave her privacy to complete the task.
When she was seated again in the chair, I told her I was going to polish her teeth first. I selected coarse prophy paste, because I did not need disclosing solution to tell me this dental biofilm was thick and adherent. I knew for certain the toothbrush would not tackle this formidable foe. I polished and flossed and had her hold a mirror to watch me floss, not only for technique but to demonstrate what it was removing and the bleeding that occurred. Then I told her I was going to use my “tools” to carefully check around each tooth to make sure I removed all of the plaque.
The whole procedure went very well, and I was queen for a moment - that is until I got her 9-year-old sister in the chair.
I proceeded as I had with the older girl, but did not expect the generalized brown stain and stained calculus the 9-year-old had on her lower anterior teeth. Just the same, I demonstrated home care, had her brush, and I polished and flossed prior to scaling. She did not like the hand scaling, and the tears in her eyes were pretty impressive, so I used the ultrasonic to complete treatment. The immediate benefit was that I had much less instrumentation to perform overall, and I ended up being accepted as their official hygienist. I treated these lovely girls into college age.
After that experience, I polished first on all children and teenagers. I discovered that this is a wonderful way to evaluate home care, show them where they are missing (without a bunch of red or purple stuff!) and reduce the scaling time significantly. This brings up another point - I completely disagree with dental offices that schedule children in the dental assistant’s chair for coronal polishing and charge for a prophy. I am amazed at the subgingival biofilm, and the gingivitis and halitosis that can result in young children! I love dental assistants, but they are not qualified or trained to evaluate and treat this. Just polishing a child’s teeth and applying a fluoride treatment is not complete patient care.
It did not take me long to observe the benefits of polishing first, so I started performing the procedure on adults as well. I explain to the patient that it helps me look around their entire mouth before I begin scaling one tooth at a time, assists me in evaluating home care, helps me focus on what cannot be removed with the toothbrush, floss, or other interproximal aid, reduces scaling time, and alerts me to possible sensitive areas. I will say, “You can be sure that all that ‘gritty stuff’ will be rinsed out of your mouth by the time treatment is complete.”
One patient, who was always apprehensive about a prophylaxis appointment, was so enthusiastic about this procedure that when she moved to a different city, she declared that she would insist her new hygienist polish her teeth first.
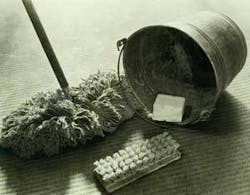
Sweeping before mopping
I have been treating an 87-year-old patient in the dental practice where I work for 11 years. She has a full dentition (30 teeth!) and less than optimal home care even though I know she tries. Despite always missing the buccals of Nos. 27-32, and food debris is usually present in the maxillary posterior areas, her pocket depths remain stable, reminding me that periodontal disease is not entirely dependent on the amount of plaque or poor home care. Disease progression needs to have that added element of susceptibility by the host.
This patient described polishing first in a wonderful way, “It’s like sweeping the floor before you scrub it.” Why would you want to mop around a bunch of loose dirt on the floor? You want that stuff out of your way so you can concentrate on cleaning the real dirt.
I sometimes feel a bit guilty that I might be removing so many microns of enamel. Shirley Gutkowski, RDH, reported in an article that while most hygiene schools teach students to use fine paste, about 50 percent of hygienists actually use coarse as their primary paste. Why is this, I wonder? Perhaps because it works better.
Terri Tillis, RDH, discussed in her course at a recent RDH Under One Roof that intact enamel is harder than the particles in toothpastes. She said enamel does not get abraded, and she likened this to scrubbing a porcelain sink with cleanser. The porcelain remains intact while removing stains and dirt. The same holds true for polishing pastes; however, it is important to remember that dentin can be abraded easily. But now that there are so many types of prophy pastes, many with benefits such as desensitizing and remineralization (such as Enamel Pro™ with amorphous calcium phosphate), routinely applying a paste might have benefits after all.
Using good judgment on when to polish
It is important to use clinical judgment and remember the philosophy of individualized patient care when deciding to polish first. Although I nearly always polish first, there are times when I do not polish at all, or polish selectively. If a patient has optimal home care and no visible plaque or stain, then I don’t polish. If I have a periodontal maintenance patient with good home care, and the periodontal condition requires the entire appointment to thoroughly debride the subgingival root surfaces, I don’t polish unless applying paste for desensitizing or localized stain removal. I may elect to selectively polish certain areas as I move through the dentition (I still scale/debride by sextant). An example is the lingual surfaces of the maxillary anteriors. When these teeth have deep, stained fissures, a prophy brush with a bit of pumice works great to remove this stain.
When is it not appropriate to polish first? An initial therapy patient who requires quadrant scaling with anesthesia would not be a candidate for polishing first. However, when this patient returns for periodontal scaling/root planing appointments, polishing and flossing the previous quadrant while he/she is getting numb is an excellent way to assess home care, demonstrate home care, evaluate for sensitivity, and apply desensitizing medicaments. After I polish, floss, and modify home care, I debride the quadrant to remove plaque, residual hard deposits or newly mineralized deposits. I proceed in this manner every time I see the patient.
Some might say that polishing is not therapeutic. I would like to present the idea that it is indeed therapeutic. What is therapy? Professional removal of dental biofilm is absolutely therapeutic. Polishing is a method of debridement that is generally not painful or invasive. Some disadvantages are the production of contaminated aerosols, but rubber cup polishing produces fewer aerosols than air-driven or power-driven scalers.
Other points for polishing first:
• Esther Wilkins reports in her textbook a disadvantage to polishing after scaling. “With the fast rotation of a rubber cup, particles of a polishing agent can be forced into the subepithelial tissues and create a source of irritation.”
So it seems logical and advantageous to polish first, because the subsequent use of power-driven and hand scalers and frequent rinsing during the hygiene procedures will rinse these particles away. An ultrasonic scaler will provide more effective irrigation, particularly subgingivally, than just rinsing with an air/water syringe.
• Wilkins also said, “Stain removal after gingival and periodontal treatments, including scaling and root planing, is not recommended on the same day.”
By polishing first on a gingivitis patient who requires only one scaling appointment, or polishing the previously scaled quadrant on a patient who requires multiple appointments for periodontal scaling and root planing, you avoid embedding particles that are out of reach from rinsing.
• Wilkins states, “Certain stains can be removed by scaling, whereas others require polishing.” Darby and Walsh state, “Because hand instruments are small, they can remove stain in areas inaccessible to a rubber cup.”
Therefore, it makes sense to remove stains with polishing first, then the clinician can focus on the remaining stains with power-driven or hand scalers. Some clinicians believe it is not important to remove stain the patient cannot see, but the
patient does see the stain! The only stains I cannot see in my mouth are on the linguals of the maxillary anterior teeth.
• I am always amazed at the plaque that polishing and flossing do not remove. This includes not only subgingival plaque, but supragingival plaque as well. There are forms of sticky plaque that do not come off with rubber cup polishing. Some of this supragingival biofilm is quite adherent and requires a scaler to remove it.
This proves to me again and again that patients cannot go it alone. They need us. Regardless of a patient’s best efforts at self-care, there are areas where plaque will be missed. The damaging effects of bacterial plaque take place below the gumline, so professional debridement/recare is imperative, and polishing first fosters taking the time and opportunity to focus on this aspect of dental hygiene care.
New dental hygiene graduates ask me how they can address the challenge of time management when they get into practice. One of the first things I tell them is to polish and floss first. When I see some of these students, now colleagues, at continuing education events, they tell me that they polish first, and they love it. A colleague who went to work in an office with 50-minute hygiene appointment times for adult patients rather than the traditional one-hour, started polishing first to help her stay on schedule. Now that she understands firsthand the benefits of polishing first, we have gotten brave enough to present the idea in the educational setting, and encourage students to “think outside the box” and use a critical-thinking process to decide when it is appropriate to polish first.
I challenge those of you who have not tried polishing first to try it for one day, and see if you observe the same benefits that I have over the past 11 years. When I see Wendy at continuing education events, I tell her what an influence she has had on me, and what I have learned about polishing first. I tell her that at school we still teach selective polishing, and now part of that is selecting the patients who are appropriate to polish first.
References
1. American Dental Hygienists’ Position Paper on Polishing Procedures. http://www.adha.org/proissues/polishingpaper.htm (accessed 28 June 2006).
2. Gutkowski S. (Nov. 2001). Whether They Need It…Or Not! RDH Magazine.
3. Wilkins EM, Clinical Practice of the Dental Hygienist. 9th ed. Lippincott Williams & Wilkins 2005.
4. Darby ML and Walsh MM, Dental Hygiene Theory and Practice, 2nd ed. Saunders 2003.