Never forget identifying signs of methamphetamine abuse
by Noel Kelsch, RDHAP
Knowing the signs and symptoms of methamphetamine (MA) abuse can save lives. As medical professionals, it is vital to know the protocol for identifying and treating patients affected by the use of this drug.
MA is a highly addictive drug. It is the second most abused illegal drug in the world, second only to cannabis. According to the Substance Abuse and Mental Health Administration (SAMHA) 2005 report, 4.9% of the population have used meth. That's 12 million people. For every 100 people we see, about five will have used meth.
MA is easy and cheap to produce, and directions are even available on the Internet! The high lasts about 12 hours; in contrast, the high associated with cocaine lasts only one hour. MA can be taken orally, rectally, optically, vaginally, or by injection. It is an effective central nervous system stimulant and gives the user a feeling of euphoria, strength, and endurance. According to SAMHA, the recovery rate from this highly addictive drug is about 5%. The life expectancy of a user is about seven years.
Many health-care professionals may think this drug is only in low income areas or metropolitan areas. But it affects every walk of life, and if you think you have no patients who use meth, I hope you read this article closely.
Her Story
I began seeing this particular patient when she was a nine-year-old, freckle-faced girl with gold hair in pink ribbons and a matching ballerina dress. She once informed me she would leave if I didn't have bubble gum flavored prophy paste. Every six months, she made me smile as I watched her evolve from braces to her first date. The years sped by, her crayon drawings lined my operatory closet, and I was thrilled when she came to me to be her mentor on career day during her junior year of high school.
But 16 hit hard. She arrived with her arms crossed, dressed in black, bangs hiding a pale, gaunt face. Her smile was absent. She announced, “I'm leaving if you lecture me.” Holding back tears, I began the assessment. I opened her mouth and saw why she warned me. She knew I would understand what was happening in her mouth. It reflected what she was doing with her life. She wanted my help and didn't know how to ask.
I went over her health history. Her temperature was 100 degrees. Her blood pressure was 145/85. Her skin was clammy and pale. The finger tips on her right hand had a brownish/yellowish cast to them. She had had angular cheilitis and ulcerations throughout her oral cavity. Her occlusal surfaces had wear facets. This sweet child who had never had a cavity in her life now had interproximal caries on Nos. 8 and 9, and demineralization with a white chalky appearance on the posterior buccals.
I said, “Something in your mouth doesn't make sense. Are you using recreational drugs or herbs?” I said it in the same tone that I would ask any other medical history question. Her eyes filled with tears and her story unfolded.
Had I asked her if she was addicted to drugs, chances are she would have said no. She did not see herself as a drug addict. The words “recreational drugs” can lead to open dialogue. I explained to her that recreational drugs mixed with dental drugs can lead to death. I showed her the oral results of her activities. My precious patient was addicted to MA.
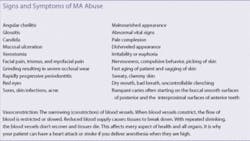
The signs of MA abuse often show up in the mouth first. Knowing the oral, social, and physical signs of MA abuse is the first step to helping patients become healthy (see table). The simple question, “Are you using any recreational drugs or herbs?” could save a life. There's no doubt this question should be on every single health history form.
Why the mouth?
MA has several properties that when combined, create an environment that destroys the teeth, blood supply, and supporting tissues of the oral cavity. The most devastating property of this drug is vasoconstriction (see table).
In the past, the rampant caries associated with MA use were attributed to the acidic nature of MA in the oral cavity when it was smoked. The current hypothesis involves a group of conditions that when combined create the perfect environment for dental disease.1 The pattern of decay is distinctive in that it initially involves the smooth buccal surfaces of posterior and interproximals of the anterior teeth. It leads to the destruction of the coronal portion of the tooth.2
MA users are unable to do daily tasks such as brushing and flossing, due to the crash effect of the drug, which can last many days. When they're awake for long periods of time, the energy bursts they experience do not allow them to concentrate on simple tasks.3
MA causes blood vessels to constrict, including those in the mouth. With repeated shrinking, the vessels will not recover, causing dental tissue to starve and break down. The result is tooth decay, gum disease, and bone loss.
The caries rate in MA abusers is four times higher than control groups.4 The dry mouth that accompanies this drug leads to many problems. Without saliva, acids accumulate, lowering the pH of the mouth and causing the breakdown of the surface of the teeth. Xerostomia is caused by the vasoconstriction and reduction of salivary gland function. The tongue and lining of the mouth can become raw and irritated without the surfactant action of saliva. This can lead to secondary infections, and limited ability to speak and eat.5
Many patients try to reduce the xerostomia by consuming sugary sodas. The soda, coupled with decreased home care, vomiting side effects, and decreased immune response, create the perfect environment for caries.
Some chemicals used to manufacture MA cause chemical burns on the skin. These chemicals also come into contact with the soft tissue or mucosal lining of the oral cavity. Without the buffering effects of saliva to protect the oral tissues, severe inflammation, painful mouth sores, and ulcers can develop. This also affects enamel.6,7
MA users are chronic grinders and clenchers due to the muscle constriction that accompanies MA use. Grinding and clenching were once attributed to the impurities of the processing in a homemade laboratory, but there is no current clinical evidence to support this.
A result of vasoconstriction is the gaunt look and quick aging of patients. Tissues of the face die and sag from the lack of nutrients and blood supply.8 This aging effect is irreparable. The intense itching that many MA users experience is from the constricting capillaries near the surface of the skin. Compulsive scratching often leads to infection and bacterial cellulitis.9
What is the next step?
The next step should be setting up a protocol for meeting the needs of the patient. You may never see this patient again after he or she has been identified. Giving patients the information they need for applying preventive measures is vital. I had a patient approach me recently and tell me the simple card that I had given him three years ago had saved his life. The card named local agencies that help with recovery. He had held it in his wallet until he reached rock bottom, then used it to change his life.
Three things to do for your patients
1. Refer them to a physician for an exam and physical. The drug can damage organs, and it's important to know what you're dealing with before a patient is in the chair.
2. If they are not in a treatment program, give them the information on local agencies. These names and numbers can be obtained from your local health department or by calling 211.
3. Ask the patient to bring their drug counselor to future appointments for pain control and treatment planning.
Oral preventive measuresXerostomia
The problem: The vasoconstriction of the salivary glands, along with the drying effects of MA agents, leave the oral mucosa severely dry. Upon examination, patients with xerostomia may complain of generalized mouth soreness, dry mouth, painful or burning tongue, taste changes, difficulty chewing, and problems with talking and swallowing. Clinical presentation of xerostomia includes oral fissuring, ulceration, and epithelial atrophy.
Preventive ideas: Saliva substitutes and moisturizers can reduce some symptoms. GC America's Dry Mouth Gel, Sunstar Rincinol P.R.N., and GlaxoSmithKline's Biotene are great products. All three have coating and healing properties and the ability to moisturize. Encourage patients to drink water or drinks sweetened with xylitol rather than trying to quench their thirst with sugary sodas, sports drinks, or fruit juices. Xylitol products reduce caries, resist the fermentation of bacteria, reduce plaque formation, and increase salivary flow.10
Decay
The problem: The results of using MA can take years to appear in the oral cavity. Patients report that their teeth decay “from the inside out.” A possible explanation may be from reduced blood supply to the teeth. With repeated shrinking, the vessels won't recover, and without nutrients to teeth, they will die. Incipient decay white spots are the result of acid exposure and lack of care. Treating carious lesions with conventional means is of little value with patients who use MA. The disease will reoccur under the filling material. Moisture problems make sealing the area with traditional materials difficult.
Preventive ideas: I strongly recommend treatment with GC America MI Paste Plus to strengthen and remineralize the damaged enamel rods. I have had success with fluoride varnish such as 3M CavityShield to coat the teeth with a protective layer when the patient is not ready for definitive treatment. Glass ionomer cements and bonding agents such as GC America Fuji PLUS can place the patient in a holding pattern and protect against the acidic nature of the drug. This product releases fluoride into the tooth for 24 months, releasing six times as much fluoride as the average sealant. It is self adjusting and can be used in one visit for patients who are not consistant with their appointments. Temporary materials can give patients a smile until the results of MA can be seen completely. Many patients end up in full mouth dentures as a result of MA use.
Oral mucosa
The problem: Oral mucosa wounds, angular cheilitis, mucositis, or Candida albicans (oral thrush) are the results of a compromised immune response and a dry, acidic environment.
Preventive ideas: Having the patient swish with a 50/50 mixture of liquid Kaopectate and Benadryl will heal and relieve pain. Rincinol is effective at coating lesions and alleviating discomfort. Evaluate the patient for Candida albicans. If present, treat oral candidiasis by prescribing either ny-statin suspensions or clotrimazole troches, both of which are effective treatments.11 Eating yogurt with live bacteria or swishing with an acidophilus tablet broken into water can balance the Candida albicans problem long term.
Grinding and clenching
The problem: Due to vasoconstriction, the muscles of the temporomandibular joint and surrounding area will constrict, leading to clenching and grinding.
Preventive ideas: Custom mouth guards are recommended but are often chewed through. Over-the-counter sports guards are cheaper and easier to replace. Some patients use a baby pacifier during this stage.
Periodontal disease
The problem: MA users do not generally seek regular dental treatment so they will often present with gingivitis or periodontitis. Vasoconstriction of the blood vessels leading to the periodontium can lead to bone loss.
Preventive ideas: Patient education on plaque control, nutrition, and the etiology of disease can help patients maintain the area until treatment. Discuss good nutrition to help tissues heal after treatment. Chlorhexidine containing alcohol should be used with caution because of the drying effects of alcohol. Chlorhexidine Gluconate Oral Rinse from Sunstar America without alcohol is very beneficial. Interdental products that are easy to use and have antibacterial properties are preferred. Multivitamins can help with nutritional issues.
Pain control
The problem: Many patients come to their hygienists for drugs, and it's important to establish if they're in pain or “doctor shopping.” A surprising thing is how some patients who look like they should be in pain due to vasoconstriction and nerve damage feel nothing. Other patients you think would have no pain have severe pain.
Preventive ideas: No patient deserves to be in pain. It's important to check each patient. You may have to ask some of them where they get their prescriptions and follow up with their pharmacist, or have their general physician work with you on pain medication. When treating after evaluation, use long-lasting anesthetics such as marcaine. Avoid narcotics due to cardiac reactions. Do not give anesthesia until the patient has not been using for 24 hours and this is well documented. Have that confirmed by his or her physician. Include the drug counselor in decisions on pain control.
Every dental hygienist has the responsibility to recognize and identify MA abuse. Adding a single question to patients' health histories can save lives.
References
1. Shaner JW. Meth Mouth and Rampant Caries in Meth Abusers, APC, Vol. 20, No. 3 p. 146-150, 2003.
2. Colfax GN. Methamphetamine -The Scope of the Problem, Medscape HIV/AIDS, 2005;11(2).
3. Zweben J, et al. Methamphetamine Treatment Project, Psychiatric of Symptoms Methamphetamine users. AM J Addict, 2005, vol. 13, p. 181-190.
4. De Cugno F, et al. Salivary secretion and dental caries experience in drug addicts. Arch Oral Bio.1981, vol.26, p. 363-367.
5. National Institute on Drug Abuse, InfoFacts: Methamphetamine (Rockville, MD: US Department of Health and Human Services), http://www.nida.nih.gov/infofacts/methamphetamine.html accessed August 4, 2008.
6. Derlet RW, Heischober B. Methamphetamine, Stimulant of the 1990s? WJM 1990, December, Vol. 153, no. 6, p. 625-627.
7. National Institute on Drug Abuse, InfoFacts: Methamphetamine (Rockville, MD: US Department of Health and Human Services), from the Web at http://www.nida.nih.gov/infofacts/methamphetamine.html accessed August 4, 2008.
8. Albertson TE, et al. Methamphetamine and the Expanding Complications of Amphetamines, WJM, April, 1999-Vol. 170, no. 4, p. 214-219.
9. Prah OPH. Methamphetamines: Are tougher anti-meth laws needed? CQ Researcher, 2005: July, Vol 15, p. 589-612.
10. Creanor SL, Strang R, Gilmour W, et al. The effect of chewing gum use on in-situ enamel lesion remineralization. J Dent Res 1992;71:1895-1900.
11. Vazquez JA. Options for the Management of Mucosal Candidiasis in Patients With AIDS and HIV Infection. Pharmacotherapy 19(1):76-87, 1999. © 1999 Pharmacotherapy Publications.
Noel, Kelsch, RDHAP, has also published a continuing education course on methamphetamine abuse that appears at www.IneedCE.com.