With prescription medications and over-the-counter drugs increasingly common, more patients are experiencing a little-known side effect: xerostomia, or dryness of the mouth. A prolonged absence of saliva can have serious effects on oral health.
magine walking into your favorite restaurant and anticipating a tasty dish. But when you open the menu, you’re dismayed to find many items are no longer available to you. You envy your dining companions as they order delicious meals and resign yourself to another bland, uneventful dining experience.
For people with dry mouth, this scenario is very real. One of the symptoms of xerostomia is an aversion to dry food.1 This means ordinary menu items such as sandwiches, steaks, or seafood dishes are out of the question. These foods can create difficulty swallowing, which can lead to potentially awkward social situations and the risk of choking from insufficiently moistened food.2 Xerostomia patients often favor soups and pastas with heavy sauces. But even these foods, which are appealing under normal circumstances, become limiting when they are the only menu options.
Xerostomia: an underdiagnosed condition
Patients consult with you about various ailments because they are confident you can alleviate their discomfort. But they may not be telling you the whole story when it comes to overall oral health. With prescription medications and over-the-counter drugs increasingly common, more patients are experiencing a little-known side effect: xerostomia, or dryness of the mouth.
Xerostomia is a common, yet underdiagnosed, condition characterized by an absence or diminished quantity of saliva.3 It currently affects the daily life and oral health of an estimated 10 percent of the population, and numbers are growing.
More medicines, parched mouths
We are a highly medicated society: 50 percent of U.S. adults take at least one prescription medication during a given week, and the numbers are higher for adults over 65.4 Advances in modern medicine mean a greater number of drugs exist to treat serious conditions that were once considered incurable. While longer life expectancies attest to the success of new drugs, medications have side effects.
With more than 400 commonly prescribed medications associated with dry mouth, it’s no wonder that approximately 64 percent of all dry mouth cases result from use of medications.1,5 As the U.S. population ages and scientific breakthroughs yield more medicines, you will likely encounter a higher incidence of xerostomia in your patients.6
Patients and antidepressants
Certain classes of antidepressants can predispose a patient to xerostomia, especially when they’re taken with other xerostomia-inducing medications.6 Depression accompanies many common medical conditions that require xerostomia-inducing drugs, such as cardiovascular disease, cancer, and neurological disorders such as Parkinson’s and multiple sclerosis. Patients who take antidepressants in combination with other medications that list xerostomia as a side effect are at a greater risk for developing this condition.
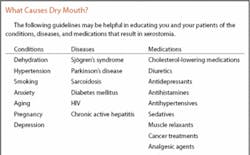
Determine the cause
Medication-induced xerostomia is a side effect found in many prescription drugs, such as cardiovascular medications (antihypertensives and diuretics), antidepressants, sedatives, antiallergens, and antacids.1 Once you have determined if a patient’s xerostomia is drug-induced or due to a health condition, you can use the information to recommend a solution. Based on your findings, you may recommend the patient consult with a physician to determine if another medication could be substituted for one causing severe xerostomia. Physicians can suggest other viable options such as gland-stimulating drugs or alternate medications.
Reviewing a patient’s medical history and current prescription drugs prior to an exam will reveal a wealth of information.6 Patients suffering from Sjögren’s syndrome, endocrine disorders, stress, or depression may experience dry mouth as a result of their condition. Serious diseases such as diabetes, HIV, hepatitis, and Parkinson’s disease also count dry mouth as a common side effect.3 Cancer patients are particularly susceptible, as radiation therapy or chemotherapy injures the salivary glands and causes temporary or permanent xerostomia.1
As a dental professional, you should be concerned and aware of xerostomia. Saliva, a seemingly simple concoction of water, proteins, and electrolytes, controls bacterial growth in the mouth, stops tooth decay, and heals wounds.4 Saliva facilitates other essential functions as well, including tasting, swallowing, speech, and digestion. A temporary reduction in salivary flow may decrease oral moisture and result in dry mouth, mild burning in the mouth, or a sensation of decreased taste. Other short-term symptoms include difficulty swallowing dry food, a need to sip water when swallowing, stale breath, and sleep interruptions due to thirst.1
While short-term symptoms are mere annoyances, a prolonged absence of saliva can have serious affects on oral health, threatening both the soft and hard tissues in the mouth.4 Decay at or under the gum line, where decay rarely develops in patients with normal salivary flow, is common among those with xerostomia. Without the antibacterial qualities in saliva protecting teeth and gums, infection can spread rapidly. Oral candidiasis, which results in white patches that adhere to mucosal surfaces, is one of the major side effects of drugs that dry the mouth, as is cheilitis, a fungal infection characterized by inflamed fissures at the corners of the mouth.
Other common complications of xerostomia include excess plaque formation and the acceleration of dental caries, or tooth decay.1 Caused by decalcification of the enamel and disintegration of the dentin by acid-producing bacteria, caries can accelerate when saliva isn’t present to clear acids and sugars from the oral cavity.3 Decay worsens when patients consume large amounts of sugary candies or beverages to stimulate salivation and keep the mouth moist.
The risk for xerostomia increases with the number of both prescription and over-the-counter medications. Consequently, older people with multiple prescriptions are more likely to be afflicted. In fact, the incidence of xerostomia skyrockets to 40 percent among elderly persons.7 Those who wear either full or partial dentures face added difficulties, particularly a greater risk of oral caries and severe denture retention problems as a consequence of decreased salivary flow. Because saliva provides part of the essential “glue” that keeps dentures in place, dryness of the mouth can cause uncomfortable shifts and make speaking and eating potentially embarrassing. Elderly persons without dentures can be at greater risk as well, since xerostomia negatively affects nutritional intake.4
Patients are often unaware that treatments exist for dry mouth, and may refrain from mentioning it during an appointment.5 Since experts estimate that a 50 percent reduction in salivary secretion is needed before xerostomia becomes apparent to dental professionals, it is possible that neither patients nor their caregivers will recognize a problem.1 For this reason, it is essential that dental professionals are aware of the medications and conditions that increase the risk of xerostomia.
Keep a regularly updated medical and dental history for each patient. Treat susceptible patients early and refer them to specialists if necessary.6 Educate patients on the importance of increased fluid intake, home fluoride applications, regular dental visits, and oral rinses that replicate salivary moistness, such as Oasis Moisturizing Mouthwash and Oasis Moisturizing Mouth Spray (GlaxoSmithKline Consumer Healthcare). These products combine polymers, humectants, and water to lock in moisture and prevent the mouth from drying out. Mouthwashes can be easily incorporated into home routines, and mouth sprays can be discreetly carried in a purse or pocket for immediate relief.
You can help identify patients who are most susceptible to xerostomia and help them develop management strategies. It’s up to you to make patients aware that the medications that make their lives better can also do irreparable damage to their teeth and gums. By sharing your expertise and discussing treatment options early, you can help patients control their xerostomia before permanent damage occurs. RDH
References
1 Guggenheimer J, Moore PA. Xerostomia: etiology, recognition, and treatment. JADA 2003; 143:61-69.
2 Mestel R. The wonders of saliva. The Oral Cancer Foundation, 2005.
3 Wilkins EM. Clinical practice of the dental hygienist. 9th ed. Baltimore: Lippincott Williams & Wilkins 2005; 387-8.
4 Ciano SG. Medications’ impact on oral health. JADA 2004; 135:1440-48.
5 Data on file, GlaxoSmithKline Consumer Healthcare.
6 Keene J, Galasko B, Land M. Antidepressant use in psychiatry and medicine. JADA 2003; 134:71-75.
7 Fox PC. Dry mouth and salivary gland dysfunction. In: Max MB, Lynn J, eds. Symptom Research: Methods and Opportunities. Baltimore: National Institutes of Health/National Institutes of Dental and Craniofacial Research, 2003.
Best Practice Tip
You can easily incorporate dry mouth assessment and diagnosis into each patient’s exam by asking the following questions:
➊ Does your mouth feel dry or uncomfortable?
➋ Do you feel like food doesn’t taste the same as it used to?
➌ Do you have difficulty swallowing dry foods?
➍ Do you constantly need to sip water, or do you wake up at night because you’re thirsty?
➎ Do you sometimes have trouble eating?
Answering yes to any of these questions may indicate dry mouth, and merit further investigation.
Nicole Greco, RDH, BSDH, is a clinical instructor at New York University College of Dentistry’s dental hygiene program. She is coordinator of the prosthodontic clinic for dental hygiene students and also focuses her efforts in the area of pre-clinic instruction, ergonomics, and instrumentation. She is a guest lecturer at NYU on case studies featuring periodontal disease and diabetes, and enjoys clinical dental hygiene. She is pursuing a master’s degree at Columbia with a strong interest in curriculum design.